Heart Matters – October 2023

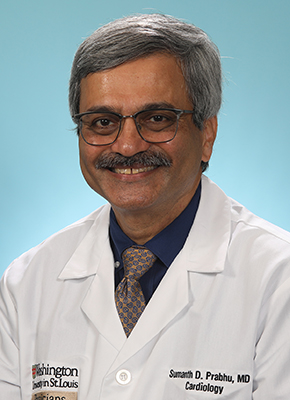
Washington People: Sumanth Prabhu

Physician-scientist integrates patient care, innovative research on inflammation in heart failure
For Washington University cardiologist Sumanth Prabhu, MD, the stethoscope is not only indispensable as a diagnostic tool but presents powerful symbolism. He sees it as a channel that connects the patient to the clinician, a conduit through which a current of information flows from the former’s body to the latter’s brain.
“When you’re a trainee, there’s this tendency to use a stethoscope strictly as a tool,” said Prabhu, the Tobias and Hortense Lewin Distinguished Professor of Cardiovascular Diseases and director of the Cardiovascular Division. “You’re trying to master what your mentors are telling you about listening to the heart. But as you become a more experienced clinician, you learn how to use the exam, how to use your patient interactions and how to integrate these together. This connection is something that you never stop learning about.”
Prabhu, who also serves as cardiologist-in-chief at Barnes-Jewish Hospital, believes that the interactions he’s had with patients have been integral to shaping his work as a researcher studying heart failure, a condition in which the heart doesn’t pump blood as it should. Most recently, his lab at Washington University School of Medicine in St. Louis has concentrated on the underlying reasons behind, and triggers for, inflammation and immune cell activation in heart failure, and on finding new therapeutic approaches to alleviate inflammation and promote cardiac repair.
“We see many patients with inflammatory responses, for example, in heart failure,” Prabhu said. “In the laboratory, we’ve studied how modulation of inflammatory responses can set the failing heart along a path of improvement and recovery. The hope is that we can eventually introduce immunotherapeutics into the clinical management of patients with heart failure.”
Even in his teenage years, Prabhu knew that he wanted to pursue medicine, mainly because the science intrigued him. However, it wasn’t until the 1980s, when he enrolled in medical school and started doing clinical rotations, that the people side of medicine drew him in.
During this time, he found himself increasingly drawn to cardiology, in large part due to the personal attention and interaction required to assess patients and their hearts. Although the physical exam is not as precise as, for example, a cardiac MRI to evaluating heart function, it yields important information that allows clinicians to interact and bond directly with patients. Prabhu began to enjoy and value that connection.
He remained a scientist, though. Prabhu went on to develop a research program in heart failure at the University of Texas Health Science Center at San Antonio and then the University of Louisville School of Medicine, after which he became chief of the cardiology program at the University of Alabama at Birmingham.
With an ever-growing expertise in cardio-immunology, Prabhu arrived in St. Louis in 2021, when he was named director of the School of Medicine’s Cardiovascular Division.
At what point did you realize that you wanted to go into the medical field?
I’m the first doctor in my immediate family, but I realized I was interested in medicine very early on, when I was in high school. I think that when you’re young, a lot of that interest is driven by the scientific aspect of the field and the cool factor of what’s possible. As you move forward, it’s really the people aspect that becomes most important. The combination of that scientific perspective as well as the personal interaction with patients — both of those things were very appealing to me.
What drew your interest to cardiology?
Even as a medical student, I was just fascinated by cardiology. I went to medical school in the mid-1980s, when the field was seeing an explosion of new treatments and approaches. There were a lot of advances with medical therapy, and it was a field that was quantitatively very precise. It was all very exciting.
In cardiology, you can be uniquely involved with both science and people in very meaningful ways. It’s very individualized, I think. I was drawn to it very early on.
What have been some of the key challenges you’ve faced in this field?
On the research side, the challenge is always getting people to believe in your work, which is a healthy challenge, developing fruitful and long-lasting collaborations, and, of course, sustaining research funding. Cardio-immunology, for example, was a newly emerging field when I first started research in this area, and there was a certain bar and burden of proof that had to be met for the scientific community to accept the validity of new observations.
In terms of scientific discovery, one of the ongoing challenges is to rely more on multidisciplinary collaborations to develop innovations that can improve the lives of patients. For instance, in our efforts to understand heart failure, we need to combine efforts with our colleagues at other institutions, developing methods to gather and analyze data — such as patient outcomes, imaging studies and biopsy results — from multiple medical centers. Doing rigorous research on a grander scale across institutions and having enough funding to do it, I think, are very important issues facing the field. That’s also not something unique to cardiology.
Is there an important moment in your career that stands out to you?
Moving my research from cardiac remodeling and signaling to cardio-immunology in heart failure was a true watershed moment. The change was at once both incremental and extreme — I wanted a broader, integrative focus looking at how immune activation is driven by both cardiac injury and organs beyond the heart. This shift in focus to cardio-immunology was the culmination of many small steps driven from grassroots research principles; it took more than five years to publish our first paper on the immune remodeling of heart failure.
On the clinical side, it was really becoming a heart failure cardiologist as a logical outgrowth of my work with patients in general cardiology. There were no prescribed subspecialty training pathways for advanced heart failure and transplantation until the 2010s, well after I completed my fellowship, so I became a heart failure subspecialty cardiologist on the job, essentially, at the University of Louisville, where my partners and I were able to develop a high-volume destination left ventricular assist device (LVAD) program. I think this is one of the defining moments for me that thematically tied together my clinical and research expertise.
What do you think we can expect from the field of cardio-immunology in the future?
I think cardio-immunology is at an important crossroads, with discoveries being made at a rapid pace in multiple scientific areas, including heart failure, hypertension, atherosclerosis and cardio-oncology. As of now, most of this remains primarily in the preclinical space. The future — the next decade or so — is bright for clinical translation, moving from preclinical discoveries to clinical trials, and then ultimately into new therapeutic approaches to help patients.
How do you maintain work/life balance?
I should have mentioned that this is the biggest challenge; it’s more of a work/life integration.
My wife, Carolina Salvador, MD, is an associate professor of medicine in the Division of Oncology here at Washington University. She also directs the Integrative Oncology and Health Clinic at Siteman Cancer Center. Our daughter is now a senior at Dartmouth. Throughout our careers, we have needed incredible time-management skills to get things done at work and outside of work to have a healthy family life.
We have tried to set clear boundaries in terms of what’s family time versus what’s work time. It is difficult, I will say, as a cardiologist and physician to do this. Our profession is very demanding with sick patients often needing urgent care. And, being a physician-scientist, there are many deadlines for projects in the research lab that also demand attention. The support of my wife and family has been most important. The ability to delegate tasks to others, and to learn to prioritize your family and mental health, are very important.
What has surprised you about the School of Medicine, and your division in particular since your arrival?
WashU is widely known as an elite medical institution. But this reputation notwithstanding, I was still genuinely surprised at the incredible level of accomplishment of our faculty, across the clinical, research and teaching domains, and the strong scholarly ethos that permeates throughout the institution. WashU is really a special place for academic medicine.
Fast facts
Where did you grow up?
I grew up in the Northeast after coming here from India when I was very young. I didn’t leave the Northeast until I was ready to do my fellowship in cardiology. At that point, I went to San Antonio, Texas, for cardiology training.
Where did you go to college and medical school?
I did combined college and medical school training in Pennsylvania. I started off at Pennsylvania State University for my undergraduate degree, and then joined Jefferson Medical College — since renamed as the Sidney Kimmel Medical College — at Thomas Jefferson University for medical school.
Where did you do your training?
I did my residency at the University of Pittsburgh, and then went on to do a cardiology fellowship at the University of Texas Health Science Center at San Antonio.
What’s your favorite thing about St. Louis so far?
My wife and I love the city and its collection of different neighborhoods. I am very happy to be back in a town that loves Major League Baseball!
Treating Ventricular Tachycardia


Every day, nearly 1,000 Americans die from sudden cardiac arrest, a catastrophic event in which the heart suddenly stops functioning. The most common cause of sudden cardiac arrest is a sustained, super-fast heart rhythm called ventricular tachycardia, commonly called V-tach. Among heart specialists, this condition is known as VT.
During VT, the heart produces irregular electrical signals that cause its ventricles, or lower chambers, to beat so rapidly that they can’t pump enough blood to the body. If ventricular tachycardia lasts for only a few seconds, the result may be a feeling of lightheadedness or breathlessness. Some people lose consciousness.
But if ventricular tachycardia lasts longer than a few seconds, the heart may stop.
“It’s important to emphasize that when most people say they feel their heart race or skip a beat, it’s very unlikely to be ventricular tachycardia,” says Phillip Cuculich, MD, Washington University cardiologist at Barnes-Jewish Hospital. “We don’t want to scare people. But what’s so difficult about this most serious of arrhythmias is that it affects both young and old, typically without warning.”
What Comes Next for VT Survivors?
Only 10% of people who experience a sudden cardiac arrest or a prolonged episode of ventricular tachycardia survive. But survivors also face new worries: What went wrong with their heart and, more importantly, can doctors prevent it from happening again?
VT typically is caused by scar tissue in the heart, Cuculich says. “For most people in the United States who develop VT, a prior heart attack has left some scarring,” he says. “Eventually, the stiff, thickened scar disrupts the heart’s normal electrical patterns and VT occurs.” Cardiac scarring can also develop in people who have had heart failure; their risk of developing VT is much higher than in the general population.
As for preventing a future cardiac arrest, that’s where an implantable cardiac defibrillator, or ICD, comes in. “An ICD is smaller than a deck of cards and is implanted underneath the skin, with leads attached to the heart that measure its rhythm,” says Cuculich. “If the heart ever goes into another life-threatening rhythm, the ICD will automatically deliver a life-saving jolt of electricity to restore a normal rhythm.”
Treating VT
For many people with ventricular tachycardia, treatment involves cardiac ablation, an inpatient procedure that uses carefully directed heat energy to create tiny new scars on the heart. These scars can avert erratic heart rhythms.
During cardiac ablation, which is performed using general anesthesia, a cardiologist threads one or more long, narrow tubes called catheters—often starting in the groin area—into a vein or veins, gently guiding them to the heart. Each catheter includes sensors on its tip that record the heart’s electrical patterns and can send controlled electrical impulses that are used to create the new, beneficial scars.
Once the catheters reach the heart, the cardiologist induces ventricular tachycardia, then uses the catheters to gather information about the heart’s electrical signals. “We need to understand where the circuitry is moving through the existing scar,” Cuculich says. “If we can find the circuit’s critical component, we can cauterize that exact location inside the heart and destroy that circuit.”
When cardiac ablation works, it tends to work very well, freeing patients from VT. But ablation can take up to seven hours to complete, and inpatient recovery can take several days. However, for many patients who undergo cardiac ablation, the procedure does not provide an effective solution, in good part because of the limitations of the technology.
“The heart can be up to 20 millimeters thick, but our catheters can only reach to 3.5 millimeters deep, meaning we can’t always send the ablative heat deep enough into the tissues to treat the circuit,” Cuculich says.
Room for Improvement
Cuculich, who specializes in cardiac electrophysiology, has devoted his career to developing safer, more effective solutions for dangerous arrhythmias like VT. “At the Washington University and Barnes-Jewish Heart & Vascular Center, we take a patient-centered view,” he says. “How can we make this better for the people we treat?”
Cuculich singles out two innovations that are available now at Barnes-Jewish Hospital, as well as a third option that is under development.
One such innovation that Cuculich and colleagues have employed is the use of an MRI scan, which is done before the ablation and used during the procedure. This noninvasive scan uses radio waves and magnets to create detailed images of the heart—including scar tissue—in two or three dimensions. “The MRI shows us where the scar is ahead of time, so we don’t spend precious minutes during the ablation to make that discovery while the patient is in VT,” he says. “We use the information the MRI offers to perform the ablation as efficiently as possible.”
Another innovative option, called electrocardiographic imaging, also produces a noninvasive map of the heart that can help guide cardiac ablation. During this imaging procedure, the patient wears a special vest containing 252 electrodes that capture electrophysiological data from the patient’s body surface while the patient undergoes a CT scan. The data from the electrodes and the scan are combined to create 3D cardiac maps.
The maps reveal crucial information about the size and shape of the patient’s heart and how it generates electricity. “When we initiate an abnormal heart rhythm in the patient, the vest of electrodes captures an immediate, panoramic picture of the heart’s electrical signals,” Cuculich says. “Within a single beat, we can visualize in detail the path the electricity takes and the shape and size of that patient’s heart, and we can discover the exact source of the arrhythmia.”
Noninvasive Cardiac Radioablation
The net result of incorporating pre-ablation MRIs and noninvasive electrode mapping, says Cuculich, is that a procedure that used to take five to seven hours now takes about three. But he believes there is still room for improvement.
“We have the scar map from the MRI, and we have a map showing the path of electricity, which means we should know where the arrhythmia is coming from,” he said. “And that should mean we can noninvasively target that area of the heart with focused radiation.”
Cuculich and Clifford Robinson, MD, a Washington University radiation oncologist, recently teamed up to develop a new approach for treating ventricular tachycardia, one that cardiologists nationwide are saying is a game-changer for patients with few remaining options. Robinson typically uses radiation therapy when he treats people with cancer at Siteman Cancer Center, based at Barnes-Jewish Hospital and Washington University School of Medicine. But he and Cuculich have shown that radiation therapy—aimed directly at the heart—can successfully treat patients with VT.
Clifford and Robinson have published several proof-of-concept studies, including one in the New England Journal of Medicine, demonstrating the promise of this noninvasive treatment for VT. As a result, the procedure will be further evaluated in an international, randomized clinical trial. Washington University School of Medicine will participate as one of the trial sites, with cardiologist Dan Cooper, MD, as the site’s principal investigator.
The treatment uses focused radiation in much the same way cancer therapy uses it to shrink tumors without surgery or chemotherapy. Cuculich says, “We have learned how to focus radiation into the scarred parts of the heart, essentially treating that area in the same manner a cancer tumor is treated.”
In noninvasive cardiac ablation, Cuculich says, a patient “lies down on the table and listens to one or two songs through headphones while the gantry—the machine that delivers radiation—moves around them, delivering focused radiation to the part of the heart that contains the scar. The patient then stands up and leaves,” Cuculich says. “This technique is turning a seven-hour invasive procedure into a noninvasive, seven-minute procedure.”
Cardiologists also are continuing to search for new ways to improve the standard cardiac ablation procedure. One potential improvement, known as multipolar mapping, involves using up to 20 sensors on the tip of each catheter. The sensors can be arranged in different formations, with the goal of capturing data more efficiently to lessen the time each patient must spend in arrhythmia during the procedure.
Another advance in treatment involves using different types of energy to ablate the heart scars. The goal in this case is to render the scar electrically inert and unable to disrupt the heart’s rhythm, says Cuculich. Other researchers have developed a catheter whose tip contains a needle. It lets the cardiologist send energy deeper into the heart muscle than a conventional catheter does.
But all these innovations are designed to improve treatment options for cardiac ablation, a treatment that finds scarred heart tissue, then uses energy to destroy parts of it. “The downside to destroying parts of the heart is that we need the heart because it sustains life,” says Cuculich. “Nobody wants to cause additional damage to the heart, but right now we don’t have other viable treatment options. We’re working toward a noninvasive treatment that doesn’t damage the heart.”
Early SGLT2 Inhibition, Spot Urine Sodium Checks May Help in Acute HF
Both approaches improved excess fluid removal, but more data are needed to determine the best strategy, Nancy Sweitzer says.

AMSTERDAM, the Netherlands—For patients with acute heart failure (HF) and signs of congestion, prompt use of a sodium-glucose cotransporter 2 (SGLT2) inhibitor or a natriuresis-guided approach to diuretic therapy both seem to be viable strategies to enhance removal of excess fluid, according to results from two small trials presented earlier this week at the European Society of Cardiology (ESC) Congress 2023.
In DICTATE-AHF, starting dapagliflozin (Farxiga; AstraZeneca) on the first day of hospitalization appeared to improve multiple measures of diuresis compared with IV loop diuretics alone, although the study fell shy of meeting statistical significance on the primary endpoint of diuretic efficiency. Importantly, it suggested that starting an SGLT2 inhibitor earlier than has been explored in prior trials is safe.
And in PUSH-AHF, using a natriuresis-guided approach to IV loop diuretic therapy—with intensification when excretion of urinary sodium was insufficient—bumped up both natriuresis and diuresis, but did not have a significant impact on clinical outcomes at 180 days.
Commenting for TCTMD, Nancy K. Sweitzer, MD, PhD (Washington University School of Medicine, St. Louis, MO), editor-in-chief of Circulation: Heart Failure, noted that both trials, though relatively small and underpowered for assessments of hard clinical endpoints, did show that the respective efforts evaluated in the studies improved diuresis. But other approaches, such as adding acetazolamide to loop diuretics, have been shown to boost fluid removal as well.
“I’m left at the end of the day wondering: what’s the best strategy to effectively diurese people? And I don’t think we know that yet,” she said. “But I will say that as a heart failure doctor, it’s fun to watch people doing diuretic trials finally because [loop diuretics are] the therapy we use in every single one of our patients and there’s been no data to guide us up till now.
There’s been no interest from the pharmaceutical industry, she added, “but it’s such an important clinical question.”
SGLT2 Inhibition for Decongestion
Zachary Cox, PharmD (Lipscomb University College of Pharmacy, Nashville, TN), who presented the results of DICTATE-AHF, noted that some small studies have indicated SGLT2 inhibitors enhance diuresis, although there have been concerns with using these agents very early in an acute HF hospitalization because of the possibility of hypoglycemia, ketoacidosis, worsening renal function, and genitourinary infections. There also have been questions about the magnitude of potential benefit.
To evaluate the impact, the researchers recruited 240 patients (mean age 65 years; 39% women) who were hospitalized with hypervolemic acute HF (regardless of LVEF), had planned or current use of IV loop diuretics, and had an eGFR of at least 25 mL/min/1.73 m2, randomizing them to dapagliflozin 10 mg daily starting on the first day of hospitalization plus structured usual care with protocolized diuretic titration or to usual care alone. IV loop diuretics were adjusted in both treatment arms to aim for a daily urine output of 3 to 5 liters.
The primary outcome was diuretic efficiency, defined as the cumulative weight change divided by cumulative dose of loop diuretics, at day 5 or hospital discharge, whichever came first. Patients in both groups lost about 4 kg in weight during that span, but the diuretic dose was significantly lower in the dapagliflozin group. Although the difference in diuretic efficiency tended to favor the intervention, it fell short of significance (adjusted OR 0.65; 95% CI 0.41-1.01).
Other measures of diuresis indicated a benefit, however, with significantly greater 24-hour natriuresis and urine output in the dapagliflozin-treated patients. That translated into a shorter time to discharge, with 52% of patients in the dapagliflozin arm and 33% of those in the control arm being discharged at the end of 5 days (P = 0.007).
In terms of safety, there were no concerning signs when looking at hypoglycemia, ketoacidosis, hypotension, worsening heart failure, genitourinary tract infections, or kidney function, Cox reported. Numbers of 30-day readmissions for acute decompensated HF or diabetes-related reasons were comparable in the two groups.
The safety is an important message because SGLT2 inhibitors are part of the foundational guideline-directed medical therapy (GDMT) for patients with heart failure and starting them during the initial hospitalization may enhance GDMT use in the chronic phase, Cox indicated. He noted that recent studies have shown that 80% of potential candidates for SGLT2 inhibitors don’t get them early on, with concerns about safety holding back use.
“This study is important in emboldening clinicians that they can safely initiate this key medication early in the hospital stay and then continue that chronically for patients with heart failure,” he said during a press conference, indicating that that would in turn have a beneficial impact on clinical outcomes.
Sweitzer said that even though there are limitations of the study, it does provide “more evidence that aggressive use of this class of agents early in hospitalization is safe.” Getting patients on a component of GDMT early in the hospital stay is attractive, she added. “It is my practice to start these drugs very early in hospitalization, so it’s nice to see additional safety data.”
Natriuresis-Guided Diuretic Therapy
Jozine ter Maaten, MD, PhD (University Medical Center Groningen, the Netherlands), who presented the results of PUSH-AHF, noted that the use of loop diuretics for the treatment of HF, the standard for half a century, doesn’t work well for a lot of patients, underscoring the need for personalized approaches to improve decongestion.
In PUSH-AHF, which was published simultaneously in Nature Medicine, the investigators evaluated whether treatment guided by periodic spot checks of urinary sodium could be the answer. The single-center trial included 310 patients (median age 74 years; 45% women) who presented with signs and symptoms of congestion. They were randomized to natriuresis-guided therapy—with IV diuretic treatment intensified based on an insufficient response, defined as a spot urinary sodium value < 70 mmol/L or diuresis less than 150 mL/hour—or standard of care.
The first primary endpoint was natriuresis, which was effectively improved with the tailored approach—the estimated amount of urinary sodium removed at 24 hours was greater by 63 mmol in that group (P = 0.0061), a difference sustained out to 48 hours. Diuresis also was significantly greater at both 24 and 48 hours.
That didn’t translate into a benefit for the second primary endpoint, however. The rate of 180-day all-cause mortality or adjudicated HF rehospitalization was 31% in both arms of the trial (HR 0.92; 95% CI 0.62-1.38). In-hospital death significantly favored personalized treatment, but overall event rates were low (two vs 14 events; P = 0.0192).
There were no differences in hospital length of stay, HF rehospitalization, 180-day all-cause death, or the percent change in NT-proBNP at 48 or 72 hours.
Natriuresis-guided treatment was safe, ter Maaten said, with no differences in serious adverse events, worsening HF, or true worsening renal function.
The approach studied here would not be difficult to implement, ter Maaten indicated, noting that spot urinary sodium values are easy to obtain, inexpensive, and widely available. “Our results furthermore underscore the use of repeated spot urinary sodium assessments for personalized treatment targets, as already proposed by the current ESC heart failure guidelines,” she said.
It might be premature to implement such an approach, however, because it’s unclear whether natriuresis guidance is better than just being more aggressive with loop diuretic therapy in general, Sweitzer said. “I don’t think we know the answer to that.”
Cardiovascular Fellow Dr. Doug Hall Featured as ACC Editor’s Pick
Third-year fellow Dr. Doug Hall contributed a piece for the American College of Cardiology’s Sports and Exercise Cardiology Clinical Topic Collection, entitled “Pacemakers and Settings in the Athlete”. Drs. Krissy Mikhova, Daniel Cooper, and Mustafa Husaini also collaborated, and the work was chosen by ACC.org Editor-in-Chief Dr. Kim Eagle as an Editor’s Pick and featured on the website’s front page.
The piece uses a quiz to challenge readers to take specifics of a case with a patient presenting with issues with their pacemaker, and determine a likely cause and course of action.

Bach and May Receive Teacher of the Year Awards
The Internal Medicine Residents of the class of 2023 voted to recognize faculty who had made a positive impact on their training. Two awards were presented for Teacher of the Year, Cardiology, during the Senior Luncheon for graduating house staff. The recipients were Dr. Richard Bach and Dr. Adam May.
This award is given to recognize exemplary leadership, patient care, and teaching. Residents felt that Drs. Bach and May provided a positive learning environment for their training. Congratulations to these outstanding educators!
Kovács Inaugurated to Hungarian Academy of Sciences

Sándor J. Kovács Jr., PhD, MD, h.c., Professor of Medicine in the Cardiovascular Division, was recently invited to Budapest to a formal inauguration ceremony for the Hungarian Academy of Sciences. Dr. Kovács was honored for his outstanding contributions in the fields of physics and medical sciences, especially in the areas of cardiovascular physiology and biophysics.
While visiting the Academy, Dr. Kovács gave an invited speech about his work and received his certification of membership as a result of being elected to the Academy for his advancement of the state of knowledge in the fields of physics and medical science.
BJC Makes Forbes’ List of Best Employers by State in Missouri and Illinois

BJC HealthCare has been named to Forbes’ 2023 list of “America’s Best Employers by State.”
BJC ranked No. 7 out of the 50 companies that made the list in Missouri and No. 29 out of 97 companies listed in Illinois.
“BJC HealthCare invests in our people by providing award-winning development programs, competitive benefits packages and a strong commitment to work-life balance,” says Keith George, vice president of talent strategy and HR operations.
“We are proud to have been recognized by Forbes as a top employer in Missouri and Illinois. Our continuous goal is to find innovative ways to support our BJC team members so they can provide the best possible care for the patients and communities we serve,” George says.
The list was based on an independent survey of U.S. employees working for companies from all industry sectors employing more than 500 employees. Forbes partnered with market research firm Statista to survey 70,000 workers at companies in all 50 states and the District of Columbia.
Participants were asked if they would recommend their employer to others, and to evaluate their employer based on working conditions, diversity, compensation packages, potential for development, company image and more. Participants also assessed employers other than their own. All surveys were anonymous to encourage candor.
The number of organizations that made the list in each state varied by the size of its companies and workforce. Ultimately, a total of 1,392 organizations across the U.S. made the list. Of those, 1,123 companies are ranked in one state only and 269 are ranked in more than one state.
You can read the full story and access the list here.
Correction- 2023 Top Doctors®
Congratulations to our many physicians recognized on the 2023 Castle Connolly Top Doctors® List.
In last month’s edition of Heart Matters, some of the 2023 Top Doctors recipients were omitted in error. The corrected list is below, including Drs. Sharon Cresci, Kory Lavine, Sumanth Prabhu, Joel Schilling, Marc Sintek, and Prashanth Thakker. We apologize for this mistake.
The Top Doctors selection process is entirely merit-based. Doctors cannot pay to be listed. More information can be found at the Top Doctors website. This list is also published every August by St. Louis Magazine.
The following Cardiovascular Division faculty have been recognized this year.
Way to Shine!
Abbott Laboratories recently recognized the excellence of the SyncAV PMT trial. Janice Amsler and Kyle Smith have been instrumental in this success.
“Janice and Kyle, this is an outstanding compliment. We are all well-aware that we have an excellent EP research team but it is awesome to hear it from a sponsor. You both work really hard to enroll patients and take exceptional care of your patients. Congratulations.”
Other Way to Shine’s for this month were Mandy Harris, Rachel Henry, Jennifer Lusk, Lizzie Tullis, the Patient Access Group, Cheryl Marshall, Barb Stehman, Dana Gima, Holley Crabtree, Morgan Porter, Nikki Depew, Emily Shaver, Nikki Madigan, Mindy Wood-Bates, and Jordan Harris.
If you catch someone in the act of shining, contact or send an email to bolhafner@wustl.edu.
CCR Spotlight: Cresci Lab

Each month, Heart Matters will highlight a research lab or clinical program. We want everyone in the division to be proud of the work we do across all of our locations and disciplines.
Since 2012, Dr. Sharon Cresci has been a principal investigator supervising her research team in the Cresci Lab. The lab uses a translational research approach to identify genetic and clinical factors responsible for variations in outcomes of treatment in cardiovascular disease, including coronary artery disease and myocardial infarction, and more recently with a special focus on hypertrophic cardiomyopathy (HCM).
Dr. Cresci is also the associate director of the HCM Center of Excellence and the Director of the Adult HCM Clinical Database and Tissue Repository. HCM is a heritable genetic condition that causes the heart muscle tissue to become thick, and can cause serious issues, including sudden cardiac death. Detection and education for people with HCM can be life-saving.
The Cresci Lab studies differences present in people with HCM and other cardiovascular diseases, to determine which biomarkers are associated with increased risk of dangerous, or even fatal, outcomes. Determining which genetic and biomarkers predict increased risks, along with genetic testing of patients with diagnosed and suspected HCM, can improve care and quality of life.
Recently Dr. Cresci received a five-year R01 grant from National Institutes of Health/ National Heart, Lung, and Blood Institute. This grant, “Determining Potential Mechanisms of Worse Outcomes in Black HCM Patients” totals almost $4 million. Dr. Cresci is collaborating with Anjali Owens, MD, Associate Professor of Medicine at University of Pennsylvania, Mike Province, PhD, Professor and Director from WashU Department of Genetics, and Nate Huebsch, PhD, from the WashU McKelvey School of Engineering.
HCM is thought to be vastly underdiagnosed in the United States, with as many as 86% of individuals with the genetic mutation that causes the disease unaware that they have the diagnosis. In Black individuals, this issue is thought to be even worse. For Black patients who are diagnosed, there are further disparities in care, including lower referral rates to Centers of Excellence and lower rates of genetic testing.
Clinical conditions that are more common in the Black US population may also exacerbate HCM and cause it to progress more quickly, such as high blood pressure. Also, high blood pressure by itself often cause the heart muscle to thicken and thus may make it harder to detect whether HCM is present on an echocardiogram, leading to missed, or later diagnosis. The grant will enable the Cresci Lab and their collaborators to study these and other mechanisms of diagnosis and treatment, to better understand potential factors contributing to overall worse outcomes for Black patients.
Dr. Nate Huebsch works with Dr. Cresci and has developed a unique engineering solution to help gain insights into how heart tissue reacts to different triggers. “Given the importance of non-genetic, mechanical factors in heart disease, we have developed micro-scale heart tissues that allow us to test both genetic and mechanical components in the pathogenesis of HCM. We are excited to work with Dr. Cresci to leverage this technology towards her studies,” Says Dr. Huebsch.
Cresci Lab members Dr. Janice Huss, a visiting researcher, and research specialist Allie Li round out the team, along with Cardiovascular fellow Cliff Pruett, MD. Though the lab is smaller than some others in the CCR, there are advantages. “We are very collaborative,” notes Dr. Cresci, “I’ve had the privilege to work with people both inside and outside the institution as well”.
Dr. Huss has collaborated with Dr. Cresci previously, when based in California at City of Hope Medical Center. She is currently working on gene and data analysis on a project studying gene expression in HCM patients, and hopes to expand into basic research approaches as well. She enjoys the collegial environment of the Cresci Lab, and says Dr. Cresci “brings people with a lot of different expertise” to collaborate on projects. “She is very skilled at bringing people together”.
Allie has been at the lab for over 15 years, and works with human blood and tissue specimens, extracting DNA and RNA, and analyzing genetic material. She thinks that the greatest strength of the lab is teamwork.
Dr. Cliff Pruett, a third-year fellow, only recently started working with the Cresci Lab, and is involved with clinical research. His current project looks at changes in the cardiac function of HCM patients after surgery. Dr. Pruett agrees that the teamwork of the lab is excellent, and “everyone’s been very helpful to get our project going”.
Meet Your Colleague

Stephanie Hicks
Lab Manager, Rentschler Lab
How long have you worked in the division? I have been with Stacey Rentschler’s lab 11 years in December, but I have been with the university for 15 years.
What is the best thing about your job? I am always learning, I love the variety of things that I get to participate in so its never a dull moment.
What do you like to do outside of work? I am very busy with my children’s extracurricular activities but when I get time I love to do Photography. I especially love sports photography. We also love to go on long hikes.
What is your favorite food? I Love Mexican food
Fun fact about you: I love to go Camping. We have managed to go on over 10 camping trips this year alone.
Division Staffing Updates
Positions open for hiring:
JR74113 Research Assistant – Dr. Rajan Sah’s Lab
JR73467 Clinical Research Coordinator II – Clinical Trials
JR72592 Research Cardiac Sonographer – Cardiovascular Imaging and Clinical Research Core Laboratory
JR73431 Postdoc Research Associate – Dr. Nate Stitziel’s Lab
JR73579 Research Specialist – Mouse Cardiovascular Phenotyping Core
JR74136 Research Opportunity – Dr. Stacey Rentschler’s Lab
JR74188 Research Opportunity – Dr. Sumanth Prabhu’s Lab
JR75743 Research Technician II – Dr. Ali Javaheri’s Lab
JR76153 Senior Scientist – Dr. Rajan Sah’s Lab
JR76174 Research Technician I – Dr. Ali Javaheri’s Lab
JR76600 Research Nurse Coordinator l – Clinical Trials
JR77127 Research Lab Manager – Dr. Sumanth Prabhu’s Lab
JR77319 Medical Secretary III – Interventional Group
JR77524 Purchasing Supervisor – Cardiology Financial Services
JR77584 Medical Assistant III – South County Practice
Welcome to the Cardiovascular Division:
Deanne Lasky, Billing Scheduling Associate I
Karen Moore, Nurse Practitioner
Cynthia Hatley, Research Cardiac Sonographer
Farewell:
Farewell to these Cardiovascular Division employees. Thank you for your service, you will be missed!
April Smith, last day with Cardiology will be 9/26
Ashley Edwards, last day with Cardiology will be 10/3
2023 Cardiology STAR Award Nominations Due October 10th
We are now accepting nominations for the Cardiology STAR Award to recognize outstanding staff members in the Cardiovascular Division. Candidates should exemplify characteristics of Service, Teamwork, Attitude, and Reliability.
Past recipients of the award include:
- Leslie Boyer – 2022
- Lisa Brinkmann – 2022
- John Murphy (Senior Scientist) – 2022
- Jessica Nigro – 2022
- Anna Ferrendelli – 2021
- Amy Gerteisen – 2021
- Amanda Gray – 2021
- Karyn Holloway – 2021
- Cortney Benson – 2020
- Diane Chapman – 2020
- Ann Mahoney – 2020
- Kaitlin Moore – 2020
- Jean Flanagan – 2019
- Erin Hoernis – 2019
- Becky Prsha – 2019
- Molly Rater – 2019
- Tonya Becker – 2018
- Gerri Cooper – 2018
- Jennifer Lusk – 2018
- Janet Schwaninger – 2018
- Craig Hunt – 2017
- Leanna Jackson-Rizzoli – 2017
- Janette Thompson – 2017
- Faith Tyler – 2017
- Linda Gallo – 2016
- Candice Jones – 2016
- Mary Wingate – 2016
- Matthew Zide – 2016
- Joan Avery – 2015
- Beth Garrison – 2015
- Margie Palazzolo – 2015
- Angie Topal – 2015
- Maria Guzman – 2014
- Anita Johnson – 2014
- Laura King – 2014
- Debbie Taylor – 2014
- Kimberly Gal – 2013
- Lori Italiano – 2013
- Katie Jennings – 2013
- Annie Nguyen – 2013
- Sharon Grimes – 2012
- Christine Kalil – 2012
- Pam Solon – 2012
- Ava Ysaguirre – 2012
We encourage you to nominate your fellow Cardiovascular Division staff member for this honor. Criteria for nominations include:
- Current staff member of 0.50 FTE or greater (minimum of 20 hours per week)
- Minimum of 3 years continuous service in the Cardiovascular Division
- Completed nomination form
- Detailed letter or description of why you are nominating the staff member
Nominations are due to Amy Borah by October 10th. Recipients will be recognized at the annual Billing Compliance Meeting on November 3, 2023.
Register for Global Health Center’s Global Health Work in Progress October Meeting
Global Health Work in Progress (GHWIP) meetings bring together members of the Washington University global health community to learn about each other’s work. Individuals working on a grant, paper or a new idea are encouraged to present their research and get feedback.
This meeting is on Monday, October 9th at 12:00pm CDT at Hillman Hall Room 120 on Danforth and Via Zoom. An exciting presentation will be given by Mitra Naseh, PhD, on
Developing a Protocol for Virtual Delivery of a Transdiagnostic Mental Health Intervention Among Afghan and Iranian Refugees and Asylum Seekers in Turkey.
This meeting will be hybrid with lunch provided to those who register and attend in person.
Registration Link: https://wustl-hipaa.zoom.us/meeting/register/tJEvc-6pqz0qEtQ6jRZBMyvnAXQRAACE9kXg#/registration
Cardio-Oncology Team at Pedal the Cause

Cardio-Oncology faculty members Drs. Zyad Qamer, Ronald Krone, and Joshua Mitchell rode for Pedal the Cause, raising money for Siteman Cancer Research.
From the Pedal the Cause website: “The mission of Pedal the CauseSM is to provide critical funding for cancer research at Siteman Cancer Center and Siteman Kids at St. Louis Children’s Hospital through our annual cycling challenge. It is our hope that research funded by Pedal the Cause will ultimately lead to a cure for cancer.”
Our Cardio-Onc team raised $2725 with their participation, and each dollar will go on to attract $12 of other funding, such as national grants. Way to go!
Tessa Carson competes in Ironman Competition

From Lisa Brinkmann:
“HUGE shoutout to our fearless leader, Tessa Carson, Executive Director of the Heart Care Institute competed in the Ironman in Chattanooga, TN on Sunday September 24, 2023.
Tessa started race day at 8:05 am with a 2-1/2 mile swim, then rode 116 miles on her bike, and finished with a 26 mile run. All that and she was still smiling as she crossed the finished line at 10:09 pm.
All of us at HCI are extremely proud of her.”
Health & Wellness
Sugar or Sweetener
Emma Greenhill, MS, RD, LDN
The World Health Organization (WHO) has released a new guideline on non-sugar sweeteners, which recommends against the use of sweeteners to control body weight or to reduce the risk of chronic diseases. The recommendation is based on a systematic review of available research which suggests that sweeteners do not help with long-term weight loss. Results also suggest that there may be potential harm from long-term use of sweeteners, such as an increased risk of type 2 diabetes and cardiovascular diseases.
In addition, added sugars in excess are also not good for our health. The American Heart Association (AHA) advises adult males consume a maximum of 37 grams of added sugar per day and adult females consume a maximum of 25 grams of added sugar per day. Each teaspoon of sugar contains about 4 grams of included added sugars. Therefore, males can have 9 or less teaspoons of sugar per day, and females can have 6 or less teaspoons of sugar per day.
This means we can still bake and cook with added sugar, but we should be limiting how frequently we add sugar and the quantity we add should be less than two tablespoons per serving. If we purchase products that already contain added sugar, then we should be smart label readers and keep our daily intake at the recommended levels.
List of common added sugars:
- Agave
- Brown sugar
- Caramel
- Corn syrup
- Honey
- Maple syrup
- Molasses
- Powdered sugar
- Rice syrup
- Sugar in the raw
- White granulated sugar
What should we do to maximize the flavor of our foods if we are advised to reduce the use of added sugars and we should sparingly choose to use non-caloric sweeteners? How do we make sweet foods taste delicious? Below are a few tips and tricks.
Healthy tricks to making foods taste sweeter:
- Add vanilla extract to plain Greek yogurt (instead of honey)
- Add cinnamon to oats (instead of brown sugar)
- Add sliced banana to corn flakes (instead of sugar in the raw)
- Add lemon juice to a marinade (instead of maple syrup)
- Add lime juice to rice (instead of agave)
- Add applesauce to baked goods (instead of molasses)
- Add pineapple to kebobs (instead of honey)
- Add shredded carrots to chili (instead of white granulated sugar)
- Add apple juice concentrate to marinara sauce (instead of sugar)
Easy Lemon Chicken Marinade

Serves: 6 • Prep Time: 10 mins • Marinate Time: 20+ mins
We love this lemon marinade! It’s incredibly versatile. Use for marinating all cuts of chicken, as well as turkey, pork, fish, shrimp, tofu, and vegetables.
Ingredients
- Zest of 1 lemon, peeled or finely grated
- ¼ cup fresh lemon juice, or the juice of about 1 to 2 lemons
- 2 tablespoons olive oil
- 1 tablespoon Dijon mustard
- ¼ teaspoon to ½ teaspoon red pepper flakes, depending on taste
- ½ teaspoon fresh ground pepper
- 3 cloves garlic, crushed with the side of a large knife or minced
- ¼ cup chopped fresh dill, parsley, cilantro, basil or a combination
Directions
- Whisk lemon juice, olive oil, mustard, red pepper flakes and black pepper together until homogenous.
- Stir in the garlic, lemon zest and herbs.
- To marinate chicken, add the marinade and chicken to a resealable food-safe bag or container and marinate in the refrigerator.
** Since this is so flavorful, even 20 minutes will work wonders. We don’t recommend marinating more than a day in advance since the lemon in the marinade can cause the chicken to toughen. **
Tips
- This recipe makes enough to marinate 2 to 2 ½ pounds of chicken.
- You can prep this marinade first, storing it in the refrigerator, before adding it to chicken as a marinade later.
- To transform into a salad dressing: To turn this into a tangy dressing, perfect for roasted or raw vegetables, increase the olive oil to 1/4 cup and whisk until blended. Refrigerate for 1 hour then discard garlic and lemon zest. Taste for seasoning and adjust with salt or add a sprinkle of sugar or a little honey to balance acidity and the mustard.
References
- Recipe courtesy of: https://www.inspiredtaste.net/27237/easy-chicken-marinade-recipe/
- https://www.who.int/publications/i/item/9789240073616
- https://www.who.int/news/item/15-05-2023-who-advises-not-to-use-non-sugar-sweeteners-for-weight-control-in-newly-released-guideline#:~:text=The%20World%20Health%20Organization%20(WHO,of%20noncommunicable%20diseases%20(NCDs).
Do you have BJC Cigna? Remember that you have annual coverage to meet with me, Emma Greenhill, a Heart Care Institute dietitian. Call 314-996-8165 for more insurance information or to schedule an appointment.
Fall well-being challenge, Walktober

Registration: Sept. 21 – Oct. 13
6-week challenge: Oct. 9 – Nov. 19
Step into autumn with WashU’s well-being challenge – a six-week opportunity to embrace the beauty of the season. Join us for Walktober, where you can track your activity, build connections, and participate on a team. Benefits-eligible employees, register online to start this wellness journey together!
Walktober Arbor Tour
October 16, 2023, from 12-1 p.m. The Offices of Human Resources and Sustainability are pleased to announce the return of the Arbor Tour, in conjunction with Walktober, the fall well-being challenge. Reserve your spot today.
Save the Date: Open Enrollment Nov. 1 – 17
Open enrollment for 2024 health and welfare benefits coverage will begin on Nov. 1 and end on Nov. 17 for most employees. More information will be communicated via email in late October regarding 2024 coverage.
For benefit help and questions, visit the Wash U HR Benefits page.
Flu Shot Information
For Wash U Employees
Getting the flu vaccine is an important public health measure to protect yourself and our community from the disease. WashU’s School of Medicine employees who work on campus or in a hybrid position at any WUSM location, including faculty, staff, and trainees, and select employees on the Danforth Campus (WUPD, Habif Health and Wellness), must receive this year’s influenza vaccination by 5 p.m. on Nov. 27, 2023, unless an employee has been granted an exemption for medical reasons or religious beliefs. You are receiving this email as you have been identified as an employee who is required to receive the flu shot as part of WashU’s 2023 influenza vaccination policy.
How to obtain your flu shot
Because the health of our community is so important, we are offering several options to get a flu vaccine:
- Multiple on-site School of Medicine flu shot clinics will be held at the Center for Advanced Medicine, 4921 Parkview Place, Suite 5A. Schedule your appointment online now. Make sure to login into ReadySet and complete your flu survey prior to attending an on-campus clinic. Please note: COVID-19 boosters will not be available during these flu clinics. Further information about future booster availability will be forthcoming from Occupational Health.
- Employees may also choose to schedule an appointment through WUCare, your primary care provider, or a local retail pharmacy to receive the flu shot.
- All options to receive the flu shot can be found at flu.wustl.edu. Please note that utilizing an external facility may result in additional incurred fees.
Flu vaccines received prior to Sept. 1, 2023, will not be accepted.
Documenting your flu shot or exemption in ReadySet
Vaccine documentation must be uploaded to ReadySet, Occupational Health Services’ secure cloud-based, electronic record-keeping database to help track flu vaccine compliance. Documentation must be submitted by 5 p.m. on Nov. 27, 2023, to remain compliant with the university’s influenza policy. Visit flu.wustl.edu for step-by-step instructions.
- If you receive your flu vaccine at an on-campus flu shot clinic, your documentation will be uploaded to ReadySet for you; however, you will still need to complete the flu survey in ReadySet.
- If you receive the flu shot off-site, through a BJC facility, or a local retail pharmacy, you will need to upload documentation yourself in ReadySet.
Any employee requesting an exemption must do so by 5 p.m. on Nov. 13, 2023. Exemptions submitted after this day and time will not be accepted. All exemptions must be renewed and resubmitted in order to remain compliant with the 2023 influenza vaccination policy. Employees who do not submit vaccination documentation or have an approved exemption by 5 p.m. on Nov. 27, 2023, will be suspended without pay beginning at 8 a.m. on Nov. 28, 2023.
Additional influenza policy information, flu vaccine FAQs, documentation instructions, exemption forms and more, can be found online at flu.wustl.edu.
For BJC Employees
BJC HealthCare has made vaccinating employees against seasonal influenza a priority every year for more than a decade.
Ongoing COVID-19 cases and changes in influenza activity since the start of the pandemic make seasonal flu vaccination particularly important as we enter the 2023 influenza season. As in past years, employees are required to be vaccinated for influenza. BJC Occupational Health will begin administering flu shots Oct. 2, and employees must be vaccinated by 5 p.m. Nov. 27.
Employees may request medical exemptions through BJC Occupational Health or religious accommodations through the HR Hub. All requests must be submitted by Oct. 1. Staff who previously received a religious accommodation must submit a new attestation through the HR Hub. Staff who previously received a permanent medical exemption do not need to submit a new request.
Vaccinations will be provided on site by Occupational Health at BJC facilities. Facilities will hold walk-in vaccination hours on specific days, and it is unnecessary to schedule a vaccination appointment in advance. Employees can receive a flu vaccination at any BJC facility during scheduled walk-in hours.
An online consent form will help speed up the vaccination process and increase efficiency. Paper forms will be available to those unable to access the online consent.
BJC Medical Plan participants also can obtain their flu shot with no out-of-pocket cost when using a Cigna participating pharmacy (for example, Walgreens) or their In-Network doctor — and by showing their Cigna medical ID card. Log in to your account at Cigna.com or call Cigna at 800-244-6224 to find a list of participating pharmacies. Employees who aren’t in the BJC Medical Plan should get their free flu shot from BJC or check with their insurance provider to understand any costs they may incur.
If employees get their vaccination outside of BJC — for example, through their physician office, a retail pharmacy or a BJC Medical Group provider — proof of vaccination must be submitted to BJCOH@bjc.org. Documentation must be in a pdf or jpg format and include two identifiers such as name and date of birth or employee ID.
Where to learn more
More details — such as how-to guides for completing and printing an online consent, FAQs and Occupational Health contact information — are available on this year’s Flu Vaccination page on BJCnet.
IT Spotlight: Phishing

How to Report Phishing to the Office of Information Security
- The preferred phish-reporting strategy at WashU is the Phish Alert Button (PAB).
- The PAB appears in all versions of Outlook (e.g., Outlook online, Outlook for MacOS, iPhone OS, Android, and Windows)
- The appearance of the PAB will vary depending on the version of Outlook you use, but in all versions, it looks like an open letter with an orange fishhook.
- If you don’t use Outlook, report phishing by sending the message, preferably as an attachment, to infosec@wustl.edu.
Ten Tips for Avoiding Phishing
- Be skeptical of urgent requests.
- Watch out for grammar, punctuation, and spelling mistakes.
- Don’t click on links in suspicious emails or open attachments you weren’t expecting.
- Keep your information private. Don’t supply log in credentials or other private information via email.
- When in doubt, pick up the phone. Call the purported sender at a known call back number (not the number the sender provided) to verify requests.
- Use secure websites and pay attention to security prompts. Look for “https://” rather than just “http://” in the Web address bar or for the small lock icon in the Internet browser but know that this isn’t a reliable indicator that the web site is safe or legitimate.
- Keep track of your data. Regularly log onto your online accounts and make sure that all your transactions are legitimate.
- Reset any account passwords that may have been compromised. If you are being prompted with DUO Push requests that you did not initiate, that means your password has been compromised! Reset it at https://connect.wustl.edu/selfservice/SECURE/ChangePassword.aspx!
- Know what’s happening. Visit the Office of Information Security page https://informationsecurity.wustl.edu/news/ often to get the latest WashU Information Security news.
- Report it. If you receive a suspicious email report it via the Phish Alert Button, to your IT department, the OIS (infosec@wustl.edu), or the HIPAA Privacy Office (hipaa@wustl.edu).
| Keep up to date with IT news at the Office of Information Security blog |
Follow the Cardiovascular Division on X!
Check out our division account, @WashUCardiology! We will be sharing division accomplishments, announcements, news, events, and more. If you have a story about the cardiovascular division that you think deserves a social media spotlight, email bolhafner@wustl.edu.