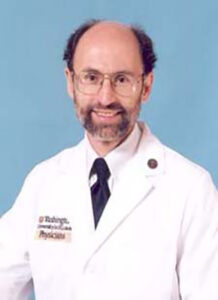
Thomas M. Maddox, MD, SM, professor of medicine and vice president of digital products and innovation at BJC HealthCare, Washington University School of Medicine, gave a presentation on new technology advances at ACC.24, the annual meeting of the American College of Cardiology (ACC). He then spoke with Cardiovascular Business, providing insights into cardiology’s future.
Maddox: Remote monitoring, AI to play key roles in the future of cardiology (Links to an external site)