Heart Matters – March 2024
Using Polypills to Transform Heart Failure Care In South Asia
From the NIH Fogarty Global International Center

Dr. Anubha Agarwal began her research in India as a Fogarty Global Health Fellow during 2017–2018, co-mentored by Dr. Doriaraj Prabhakaran, executive director of the Centre for Chronic Disease Control (CCDC) in India, and Dr. Mark Huffman, professor of medicine and co-director of the Global Health Center at Washington University in St. Louis (WUSTL), Missouri. During her Fogarty year, she developed, implemented, and evaluated, using an interrupted time series design, a heart failure quality improvement intervention including discharge checklists, audit-and-feedback mechanisms, and patient education among 1,400 patients hospitalized with heart failure in eight hospitals in Kerala, India.
Today, she is an assistant professor of medicine and co-director of the Global Cardiovascular Health program at WUSTL. Agarwal received a Pathway to Independence award from the National Heart, Lung, and Blood Institute (NHLBI) in 2022, allowing her to build on her previous research to improve heart failure care in South Asia. She aims to substantially simplify heart failure management for patients with heart failure with reduced ejection fraction (HFrEF, the type of heart failure in which the left ventricle loses its ability to contract normally, and the heart can’t pump with enough force to push blood into circulation). Her goal is to shift the treatment paradigm from a multi-drug therapy to a polypill containing several guideline-directed medical therapies for HFrEF in one pill.
Her research still in its early phases, Agarwal and her team have already conducted in-depth interviews and focus group discussions with cardiologists, pharmacists, nurses, and patients throughout India aiming to understand the current context of heart failure care and acceptability, appropriateness, and feasibility of an HFrEF polypill implementation strategy. The next phase will be a multi-center type 1 hybrid randomized clinical trial among patients with HFrEF in South Asia. It will investigate whether an HFrEF polypill implementation strategy can improve key clinical outcomes compared to usual care. Through the development, implementation, and evaluation of HFrEF polypills, Agarwal hopes to improve heart failure care in South Asia and beyond.
When asked about her motivation for this research, she states that she chose to pursue cardiology after her grandfather, who lived in India, died of a heart attack in his early 50s. She says, “It inspired me to become a cardiologist and, in many ways, inspires my continued commitment to improving cardiovascular care in India and South Asia.” As a part of the Indian diaspora, having left India at only five years of age, she adds, “It’s been incredibly rewarding professionally and personally to be a part of a team generating evidence-based research to improve cardiovascular care in India.”
Beyond her clinical and research pursuits, Agarwal embraces the role of a mentor, particularly for aspiring female researchers in cardiovascular medicine and global health science who are often underrepresented in both fields. “I have been so lucky to have been surrounded by fantastic feminist mentors who have always elevated me, and I’m trying to give that back.”
As she continues her work in India, as a part of the Indian diaspora, she wants to ensure there’s an equitable partnership that builds capacity with Indian researchers and institutions to ensure all voices are heard, “While we’re helping to train the research workforce of India, we also need to acknowledge how much we have to learn from them.”
Black People Have the Highest Rates of Death From Heart Disease. Could More Black Cardiologists Help?
Dr. Zainab Mahmoud contributed to this article by NBC News

For Elston Harris, heart attacks seem to be a generational curse.
Several men from his father’s side of the family — including Harris’ uncles — died from heart attacks. Harris, who is 59 and a former college basketball player, almost experienced a similar fate after his own heart attack in 2017. The only signs he was having a heart attack that he noticed were “small” symptoms of back pain and trapped gas.
For Harris, the curse may have been a blessing in disguise: While being treated at Advocate Trinity Hospital, a medical center in southeast Chicago, he was referred to Dr. Marlon Everett, a cardiologist who gave him a “game plan” to follow. This included putting God first, eating healthy and concentrating on his checkups. But aside from Everett’s expertise, Harris said he felt comfortable because Everett looked like him.
“When you are African American or Black, you’re more comfortable interacting with someone who knows, ‘OK, he might have grew up here, or he might eat this, or I heard them do that,’” said Harris, who lives in Chicago. “So, you’re a lot more comfortable with people who walk in similar footsteps.”
Around 60% of Black American adults have heart disease, and heart disease death rates are highest among Black Americans compared to other racial and ethnic groups, according to the American Heart Association.
Yet Harris’ experience of having a cardiologist who looks like him is a rarity. A 2021 report by the Association of American Medical Colleges found that only 4.2% of cardiologists are Black. An earlier study, published in 2019 in the journal JAMA Cardiology had similar findings, revealing that Black doctors made up only 3% of the cardiologist workforce. That same report found that 51% of cardiologists were white and 19% were Asian.
‘A sense of comfort’
For many Black patients, having a Black cardiologist creates feelings of trust and comfort, which is sometimes a challenge due to the medical system’s history of racism and mistreatment toward Black patients.
Nikita Oxner first saw Branch last year after doctors discovered she had a heart murmur that they detected during a sleep study. Oxner, 45, said up until that point, she had never sought care from a cardiologist, and even being referred to one was “scary.” Yet her fears subsided when she met Branch.
Under Branch’s care, Oxner discovered she had a condition that makes it difficult for the heart to pump blood.
Heart-related problems run in Oxner’s family. In 2019, hypertension led to her brother’s sudden death at age 31, and her grandmother died from heart disease at age 77. Her father, who died from cancer at age 39, “had hypertension, high blood pressure a majority of his life,” she said.
Oxner said that when she shared details about her brother and other family members to Branch, “she instantly understood.” While she “didn’t feel good” about having surgery to insert a defibrillator in her heart, Oxner trusted her doctor’s opinion.
“She had a lot of compassion,” said Oxner, who lives in Greensboro, North Carolina. “She was very understanding, down to earth and relatable — and really helped me understand how this could change my life.”
As a Black woman who often has to advocate for her health, Oxner said the fact that Branch was also a Black woman “mattered to me.”
Branch said the added layer of trust and comfort often seen between a Black patient and Black doctor can help motivate patients to stay on their heart medications and stick with healthy lifestyle changes.
For example, “hypertension is a big thing in our community,” she said. A Black cardiologist may also be on hypertension medication, she said, “so, they can relate and connect in that way.”
Like Oxner, Kia Smith, 42, is another Black woman who sought cardiac care from a Black physician. Smith, who lives in Ellenwood, Georgia, said she saw Dr. Camille Nelson, a cardiologist at Atlanta Heart Associates, in 2020 after experiencing an elevated heart rate. Smith said she believes that if she had chosen a non-Black cardiologist, she may have been treated like “a dramatic walk-in” and had her symptoms dismissed.
“At every turn, when I was concerned, she did not dismiss my concerns or my personal experiences,” Smith said of Nelson. “She also explained the science of everything to me, and we were able to get to a place where I was confident that I was going to be OK.” Nelson said that Smith’s symptoms may have stemmed from stress and recommended workout routines to get her heart into a healthier state.
Dr. Zainab Mahmoud, a cardiologist and instructor of medicine at Washington University in St. Louis, said many Black women tell her that they feel heard and understood under her care. Having a provider who can understand a Black patient’s experiences “creates this kind of trust and improves a patient-provider relationship,” she said.
“They’re more likely to then have their family members come or their family and friends come to see me as well,” Mahmoud added. “I’ve seen that happen multiple times I can’t even count.”
Read the whole article here.
Husaini Featured During Men’s Health Segment on KSDK News

Dr. Mustafa Husaini, Assistant Professor of Medicine and Director of Sports Cardiology in the Cardiovascular Division, was recently featured in a segment on KSDK news for Heart Month.
Today in St. Louis’ Rene Knott, Paul Cook and Anthony Slaughter spoke with Dr. Husaini about the importance of exercise in heart health, and specifically in men.
View the video here:
Monitoring Men’s Health: Cardiologist answers our heart health questions | ksdk.com
Lasala Receives 2024 Miami Valves Lifetime Achievement Award

Dr. John Lasala, Professor of Medicine and Director, Structural Heart Disease in the Cardiovascular Division, was presented with the Lifetime Achievement Award at this year’s Miami Valves annual international structural cardiology conference hosted by the International Medicine Institute of the University of Miami Miller School of Medicine.
Dr. Lasala was honored for his research, clinical and teaching accomplishments.
He gave a presentation on his 34-year career, “From Utility Baseball Player to Structural Interventionalist: A Life’s Journey,” adding that he still enjoys sports and is a consultant to the St. Louis Cardinals and St. Louis Rams.
“Miami Valves is a great way to catch up on what’s happening with valvular disease,” he added. “It’s large enough to get the latest information yet small enough that you can talk individually with other professionals.”
Congratulations to Dr. Lasala on this well-deserved recognition!
Mahmoud Appointed to ACC Reproductive Health & Cardio-Obstetrics Section Leadership Council

Dr. Zainab Mahmoud was recently appointed to a 3-year term on the leadership council of the Reproductive Health & Cardio-Obstetrics Section of the American Academy of Cardiology. Her term begins in April, 2024.
From the ACC website:
The creation of this Section addresses the needs and gaps in care in all domains including clinical care, education, training/mentorship, research, engagement and public policy. The Mission of this Section is to provide members with knowledge in a structured and organized approach on the cardiovascular care of patients surrounding all aspects of pregnancy and reproductive health; create actionable and accessible knowledge for members of the College; enhance the training of FITs by encouraging incorporation of these topics into their didactic curriculum; and lead advocacy efforts to improve care and accessibility to care for our patients. This Mission aligns with our goal to advance the value and equity of cardiovascular care for patients’ health during and around pregnancy and across the reproductive years.
Congratulations to Dr. Mahmoud on this achievement!
Rich Receives BJH Neville Grant Award
Professor of Medicine, Associate Program Director for Cardiovascular Research and
Director of the Barnes-Jewish Hospital Cardiac Rapid Evaluation Unit Dr. Mike Rich has been selected for The Neville Grant Award, the highest clinical honor bestowed by BJH, in recognition of the following traits:
1. The delivery of superb clinical care
2. Exceptional compassion for patients and their families
3. Extraordinary respect toward colleagues and other caregivers
4. Mentorship of house officers and medical students in those professional and personal qualities embodied in an exemplary physician
The award will be given on April 11th at the Semi- Annual Medical Staff Association meeting at 5:30 in EPNEC.
Jimenez Among 2024-2025 CTRFP Awardees

Washington University Institute of Clinical and Translational Sciences (ICTS) and The Foundation for Barnes-Jewish Hospital awards 20 investigators as part of the 17th annual Clinical and Translational Research Funding Program (CTRFP). The CTRFP is the largest internal grant funding program of the ICTS. Applicants are required to submit proposals for projects that promote the translation of scientific discoveries into improvements in human health. For 2024, awards were considered across three project categories: clinical/translational, community-engaged research, and biostatistics, epidemiology, and research design.
This year the CTRFP received around 70 letters of intent and awarded approximately $1M for investigator-initiated projects. These grants are supported with funding from the ICTS, The Foundation for Barnes-Jewish Hospital and ICTS partner institutions: Saint Louis University and the University of Missouri-Columbia.
Jesus Jimenez, MD, PhD of the Washington University School of Medicine Cardiovascular Division has been awarded for “Advances in the Diagnosis of Immune Checkpoint Inhibitor Myocarditis”:
Immune checkpoint inhibitors, which work by activating the immune system to target and kill cancer cells, are increasingly being used to treat patients. Unfortunately, these drugs may cause serious side effects in the heart including life-threatening myocarditis. The current approach for diagnosis is to obtain an endomyocardial biopsy. This proposal seeks to perform the first-in-patient CCR2 molecular imaging to identify patients with immune checkpoint inhibitor myocarditis. The use of noninvasive CCR2 radiotracer imaging may identify inflammatory cells to improve diagnosis of immune checkpoint inhibitor myocarditis and has the potential to track response to therapy in the long-term.
Keep up to date with all Division news on our news page!
Way to Shine!
“Sharon (Roane), Demetres (Jones), and Emily (Shaver),
I just wanted to thank you 3 for the amount of time and work you put in to get the new patient referral WQ completely empty (down from 200+ last week). I honestly did not think that was going to be possible any more. I cannot thank you enough!!
Keep up the great work!”
Other Way to Shine’s for this month were Tori Menning, Katherine Ramsay, Megan Hangyal, Deana Wilmesher, Anne Yoggerst, Lauren LaRose, Gina Bliss-Braymer, Ryan Gilliam, Karen Moore, Barb Stehman, Dana Gima, Cheryl Marshall, Sylvia Kimani, Melissa Lovell, Jenifer Abbas, Tonya Becker, Kathleen Cross, Matthew Falkinburg, Angela Higgins, Craig Hunt, Joan Krull, Angie Smith, Stephen Tepen, Katie Wehmeier, Jill Taake, Millie Cova, Jennifer Lusk, Rebecca Menley, Anita Johnson, Donna Fuehne, Aida Loera Acosta, Ann Mahoney, Kinsey Walker, Janelle Larson, Chelsea Just, Paige Rama, Noah McBride, Anna Ferrendelli, Catherine Cofield, and Lisa Ford.
If you catch someone in the act of shining, contact or send an email to bolhafner@wustl.edu.
CCR Spotlight: Dr. Rajan Sah’s Lab

Each month, Heart Matters will highlight a research lab or clinical program. We want everyone in the division to be proud of the work we do across all of our locations and disciplines.
The Sah Lab, led by Rajan Sah, MD, PhD, studies ion channel signaling in numerous different cellular contexts to identify novel approaches to treat cardiometabolic disease, including heart disease. Dr. Sah joined the Washington University Cardiovascular Division in 2018, after previously establishing a lab at the University of Iowa, where he first became interested in how studying electrical signals in fat cells from a newly discovered ion channel affected fat cell growth. Overtime, this initial research direction expanded into numerous other areas, beyond the more typical heart and vascular cells commonly studied by cardiologists to generate ideas and questions about treating metabolic issues and other problems associated with heart disease that arise in other parts of the body.
The lab focuses mainly on studying an ion channel called SWELL1 or LRRC8 that responds to swelling within a cell. They have used electrophysiology, gene-editing techniques, cell biology, structural biology, super-resolution microscopy, mouse model research and medicinal chemistry to study LRRC8 signaling in many different tissues and cell types. For example, in fat cells studying obesity, pancreatic beta cells studying insulin secretion, and endothelial cells studying vascular function. Dr. Sah hopes to continue to follow the science where it may lead to more questions and more avenues for discovery within this area of research.
In order to further support this research with NIH grants and facilitate and accelerate translation of novel discoveries at the bench to innovative therapeutics at the bedside, Dr. Sah founded Senseion Therapeutics Inc. Dr. Sah explains that the goal is to develop drugs that target specific functions, based on their findings about LRRC8 composition and signaling in each cell type.
The target, he says could be “even beyond metabolic. It could limit damage from stroke in the brain, there are also anti-platelet effects relevant to heart attack and other vascular diseases”. Although the science for this is still developing. “The biology is evolving rapidly, and it is driving the pharmacology, and vice versa.”, he says.
The Sah Lab is constantly bustling with activity, as the lab members keep very busy with their work. Lab supervisor Litao Xie has been working with Dr. Sah since he first established a lab in Iowa in 2013. She says she is known as the “mom” of the lab, and finds the work very rewarding, especially working with the mice and getting results from experiments. Instructor in Medicine Dr. Ashutosh Kumar has also been with the group since before the lab came to Wash U. He currently works on skeletal-muscle and metabolic signaling.
Yongmei Feng, a research tech, assists with molecular biology and mouse studies, as well as molecular cloning. Senior scientist Dr. Rahul Chadda is a microscopist and builds and maintains microscopes for the lab, while performing challenging single-molecule imaging studies. Postdoc John Tranter focuses on studying LRRC8 in platelet cells.
Several lab members, including staff scientist Tarek Mohamed, research techs Ryan Mikami and Nihil Abraham and postdoc Yonghui Zhao are focused on electrophysiology, measuring electrical currents in the cells they are studying and using small molecules to block channels to understand how LRRC8 channels signal and how to develop possible therapies. Nihil, who has been with the lab about six months says that “everyone is really open to teaching. If one person knows how to do an experiment, then everyone will know how to do it”.
Dr. Kumar echoes this sentiment, noting that “if someone needs to get help, everyone wants to help. Everyone can collaborate with a project, not just the main person assigned.” It’s very clear that the culture in the Sah Lab is one of mutual respect, curiosity, and collaboration.
Division Staffing Updates
Positions open for hiring:
JR79614 Research Administrator – Global Health
JR80153 Research Cardiac Sonographer – CORE LAB
JR72592 Research Cardiac Sonographer (PRN) – CORE Lab
JR77820 Clinical Specialist PT/OT (PRN) – Clinical Trials
JR80511 Clinical Nurse Coordinator – General Cardiology and Hypertrophic Cardiomyopathy Center
JR80574 Registered Medical Assistant III – NWT
JR79636 Senior Department Accounting Assistant – Purchasing Team
JR80348 Medical Assistant III – West County Practice
JR80032 Clinical Research Coordinator I – Clinical Trials
JR80321 Research Opportunities – Dr. Prabhu’s Lab
JR78663 Research Opportunities – Dr. Rentschler Lab
JR80555 Staff Scientist – Sah Lab
JR78795 Postdoctoral Research Associate – Dr. Stitziel’s Lab
Welcome to the Cardiovascular Division:
Kesha Hanks – Clinical Research Apprentice – 2/1/2024
Emily Titzer – Research Nurse Coordinator I – 2/1/2024
Joshua Sullivan – Clinical Research Coordinator I – 2/7/2024
Yuqian Xie – Research Tech I – Dr. Rentschler’s Lab – 3/1/2024
Farewell:
Farewell to these Cardiovascular Division employees. Thank you for your service, you will be missed!
Li He – 2/16/2024
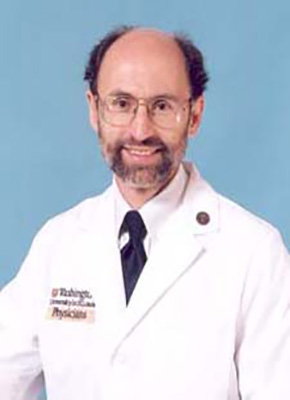
Obituary: Alan Neal Weiss, MD, FACC
In loving memory of Alan Neal Weiss, MD, FACC
10/14/1941 – 02/05/2024

Dr. Alan Weiss, esteemed clinical cardiologist and retired Professor of Medicine at Washington University School of Medicine, passed away February 5th, 2024. Dr. Weiss began his medical journey as an intern at The Ohio State University Hospital and medical resident at Barnes Hospital, where his talent and dedication shone brightly. He completed his cardiology fellowship at the University of California, Berkeley in San Francisco. In 1972, under the mentorship of Dr. Carl Moore, he was chosen as chief medical resident at Barnes Hospital, marking the beginning of his remarkable career in St. Louis, where he dedicated over 40 years of service as a master clinician. As faculty at the Washington University School of Medicine, he rose through the ranks from Assistant Professor in 1973 to Full Professor of Medicine in 1993 until his retirement in 2021.
Universally loved and respected by his patients and their families, Dr. Weiss was a beacon of compassion and expertise in the field of cardiology. His impact extended far beyond St. Louis, as he became a trusted source for referrals across the Midwest region and beyond. Dr. Weiss’s commitment to patient care led him to perform outreach at multiple sites in southern Illinois and Missouri throughout his career and to establish one of the largest clinical practices in academic cardiology. Dr. Scott Nordlicht said of Dr. Weiss: “Renowned for his diagnostic acumen and unparalleled bedside manner, Dr. Weiss was a true master in the field of cardiology. His physical examination rounds at Barnes Hospital were legendary, inspiring countless medical trainees.” Dr. Craig Reiss added “Alan helped form me into the person and physician I am today. He taught me how to approach life and the art of healing.” Above all, Dr. Weiss always prioritized his patients’ well-being and was a vocal advocate for their care. His compassion and leadership in patient advocacy set a standard for the medical community.
An additional notable aspect of Dr. Weiss’s career was his care and counsel for the greatest rabbis from Israel, who sought his expertise in cardiology issues affecting their congregations. His willingness to share knowledge and provide guidance to leaders in the community exemplified his dedication to serving others.
Dr. Alan Weiss’ legacy will live on in the countless lives he touched and the profound impact he made in the field of cardiology. He will be deeply missed and fondly remembered by all who had the privilege of knowing him. Dr. Weiss is survived by his wife, Marcia, their 3 children Mendel, Rachel, and Sarah, 16 grandchildren, and 6 great-grandchildren. A private burial in the Har Hamenuchos cemetery in Jerusalem is planned by the family.
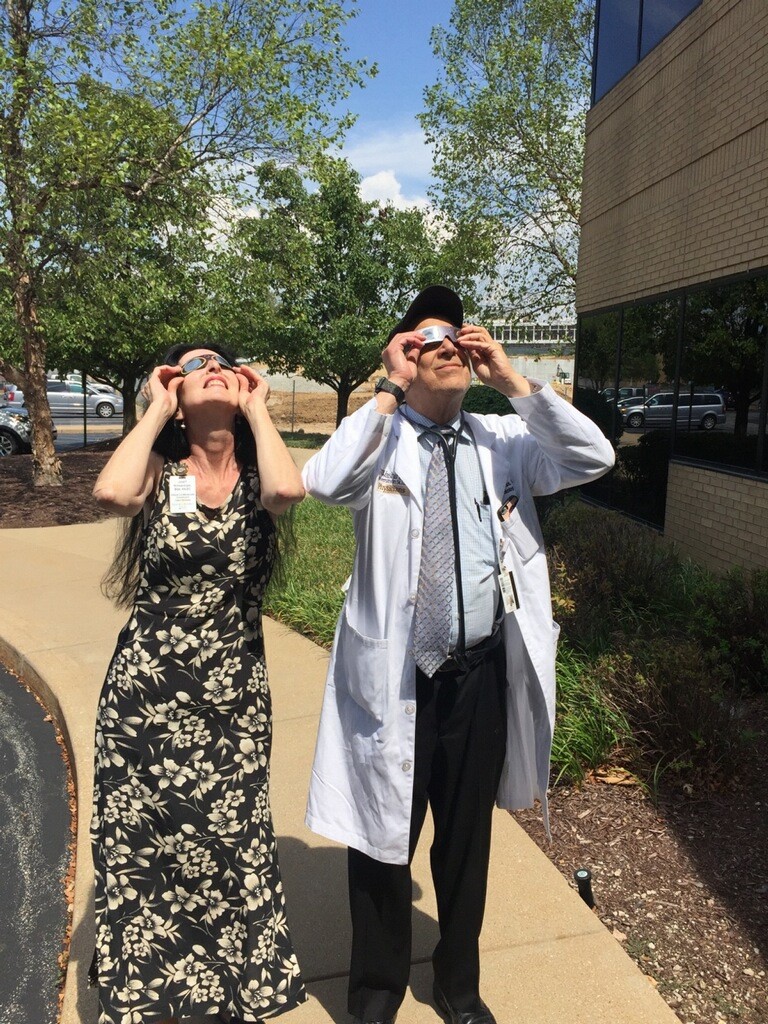
Here are some memorable photos of Dr. Weiss over the years.



Health and Wellness
Prebiotic Fiber
Emma Greenhill, MS, RD, LDN
There are many health benefits associated with eating enough fiber—it can lower cholesterol levels, and decrease the risk of type 2 diabetes, metabolic syndrome, and cardiovascular disease. Yet, only about 5% of Americans meet the daily recommended intake of dietary fiber.
Recent research. In recent years, nutrition research has begun to pay more attention to the gut microbiome. More than 5,000 research articles have been published over the past six years, supporting the influence of the gut microbiota on the entire body. Moreover, it has been revealed that a specific kind of fiber, prebiotic fibers, feed our microbiome.
Where does fiber come from. Dietary fiber includes the parts of plant foods—mainly fruits, vegetables, whole grains, nuts/seeds and legumes—the body can’t digest or absorb. It passes mostly intact through the stomach and small intestine on its way to the colon, where it may or may not be broken down by gut bacteria in the colon.
Two kinds of fiber. Terms and categories of dietary fiber have evolved over the years. Dietary fibers are categorized based on differences in solubility, viscosity, fermentability, and prebiotic properties.
Insoluble fiber. Insoluble fiber remains mostly intact in water; therefore, it is not a source of calories. Derived from plant sources, it benefits the digestive system by adding bulk to the stool and preventing constipation.
Soluble fiber. Soluble fiber dissolves in water to form a gellike substance that is thick and viscous. Viscous fibers slow the digestion and absorption of nutrients, which creates satiety, possibly reducing caloric intake and leading to weight management.
Fermentable fiber. Fermentability refers to whether a fiber is digestible by microorganisms. Most fermentable fibers are soluble, but there are some fermentable insoluble fibers, including resistant starches. Fermentable fibers slow digestion and increase satiety, which may help with diabetes management by increasing insulin sensitivity and decreasing glycemic response.
Prebiotic fibers. Prebiotic properties of different fermentable fibers uniquely benefit the microbiome by feeding the microbiome. Food sources with prebiotic properties include chicory root, garlic, leeks, onions, asparagus, and bananas. These prebiotic fibers help improve digestion, relieve constipation, improve fat digestion, and promote the growth of beneficial bacteria while preventing harmful bacteria from growing.
Palak Paneer (Spinach Paneer)

Serves: 2-3 • Prep Time: 15 mins • Cook Time: 30 mins • Total Time: 45 mins
Ingredients
- 1 ¼ cups paneer (150 grams Indian cottage cheese)
- 3 ½ to 4 cups palak (100-120 grams baby spinach)
- 2 Tablespoons oil
- 2 green chilies (deseeded)
- ¾ cup onions, finely chopped (90 grams, 1 small onion)
- ½ cup tomatoes, chopped/pureed (2 small)
- ¾ teaspoon garlic, minced
- ½ teaspoon ginger, minced
- 8-10 cashews
- ½ to ¾ teaspoon garam masala
- ½ teaspoon kasuri methi (dried fenugreek leaves) (skip if you don’t have)
- ¼ cup water (to blend spinach)
- ¾ cup water (to cook gravy)
- 3 Tablespoons cream (optional)
Directions
- If using baby spinach use the whole leaf (is using mature spinach pluck only young and tender spinach leaves and discard the stems).
- Add them to large pot of water. Rinse them well few times & drain to a colander.
- Allow the water to drain completely.
- Heat half tablespoon oil in a pan. Saute green chilies, cashews, and spinach for 3-4 minutes until leaves wilk off thoroughly and raw smell of spinach has gone away. (Another option: Blanch spinach in 4 cups hot water with ¼ tsp salt for 2 minutes. Then immerse in an ice cold water bath. Drain completely.)
- Cool this completely. Blend this along with water to a smooth puree. The puree should be smooth and thick. You may add 1-2 tablespoons more water to help with blending.
- Heat remainder of oil in same pan of low heat. Add any desired seasonings (optional: cardamoms, cloves, cinnamon stick).
- When the spices begin to sizzle, add onions and saute until they turn transparent to golden.
- Add garlic and ginger and saute an additional 1-2 minutes or until fragrant.
- Then add tomatoes and optionally flavor with salt and pepper.
- Add garam masala and saute for 2 additional minutes.
- Pour water and cook covered until onions are completely soft. (There should be some water left in the pan.)
- Lower the flame, add kasuri methi and pureed spinach. Mix well and cook until it begins to bubble for about 2-3 minutes. If the curry is too thick you may add a few tablespoons of hot water.
- Avoid overcooking. Add paneer and mix well. Turn off heat, and optionally garnish with cream.
Tips
- Serve palak paneer with naan, roti, chapati, basmati rice, or Jeera rice.
- This recipe can be doubled.
- If desired, you can substitute cashews with 7 blanched almonds or 2 tablespoons almond flour.
- Whole spices are optional. If you skip them, add more garam masala to taste.
- If using store bought paneer, then cube and add to 2 cups hot water. Immerse for 10 minutes total. Drain and use (prevent overcooking).
References
- https://www.todaysdietitian.com/newarchives/AS20p24.shtml
- https://www.indianhealthyrecipes.com/palak-paneer-recipe-easy-paneer-recipes-step-by-step-pics/
Do you have BJC Cigna? Remember that you have annual coverage to meet with me, Emma Greenhill, a Heart Care Institute dietitian. Call 314-996-8165 for more insurance information or to schedule an appointment.
Join the Division AHA Heart Walk Team!

2024 Metro St. Louis Heart Walk will be held June 1st. This event helps raise funds for the American Heart Association. From their website:
“We’re a relentless force! Now imagine how much stronger we’ll be working as a team! Heart disease is still the no. 1 killer and stroke ranks no. 5 in our nation.
We are walking together – not only for our own health, but also for yours. And for the health of our parents, our children, and our grandchildren.
The Heart Walk is a time of celebration, joy, and inspiration. It’s also an event where people work together to support one single goal – to create a world free of heart disease and stroke.
This year, the American Heart Association’s centennial is a celebration of the of the lifesaving achievements and shared vision for a bold second century that will exponentially advance heart and brain health.
Be a relentless force. Be a supporter of critical research. Be a lifesaver. Be a part of an unstoppable team. Join us now and walk to save lives.”
Join or donate to the Cardiovascular Division team, the Wash U Heart Throbs here!
Take Care Health Fair on the School of Medicine Campus March 12

At the Take Care Health Fair, you can explore resources that support the 8ight Ways to Wellness principles, discover benefits available to WashU employees, and embark on a journey to empower yourself in achieving your well-being goals today and in the future. Whether you’re seeking better health, balance, or personal growth, we have something to support every individual in our WashU community.
The Take Care Health Fair will take place in person on Tuesday, March 12, 2024, from 10 a.m. to 3:30 p.m. at Eric P. Newman Education Center (EPNEC) on the School of Medicine Campus.
Join us on campus for a variety of well-being activities, including:
- On-site health screening event (appointments encouraged)
- Fitness assessments from WashU Physical Therapy
- Tasty treats and behavior change guidance from the MyWay to Health team
- Kickoff for the spring wellness challenge
- Connect with WashU’s UnitedHealthcare Nurse Advocate, Bridgette Sims, RN
- Learn about WashU’s Live Near Your Work benefit
- FREE chair massages
- Attendance prizes, and more!
Participants can also visit with representatives from university departments and vendors including TIAA, UnitedHealthcare, WashU Psychiatry, and WashU Audiology. Don’t miss out on this excellent chance to connect with a wide array of well-being resources and gather valuable information. It’s an incredible opportunity to enhance your knowledge and take advantage of all the great insights available to support your well-being journey. Join us and explore the wealth of information waiting for you!
Medical Campus Road Work Update:
March 20 – 25
Contractors will continue the utility work in northbound Kingshighway, which was started last month, in five consecutive days versus six weekends as originally planned. This will reduce the ongoing disruption and provide a safer environment for the workers.
8 p.m., March 20 through 6 a.m., March 25
This will once again entail a lane shift for northbound Kingshighway traffic at Barnes-Jewish Plaza into one southbound lane. Impacts include the following:
- Northbound drivers will be able to turn right from Kingshighway onto Barnes-Jewish Plaza.
- Barriers will separate northbound from southbound traffic lanes, starting south of Barnes-Jewish Plaza.
- The barriers will prohibit left turns from Kingshighway onto Barnes-Jewish Plaza and Hospital Dr. (Hospital Dr. enters Forest Park across from Barnes-Jewish Plaza.)
- The traffic signal at Kingshighway and Barnes-Jewish Plaza will be turned off to keep northbound and southbound traffic moving to prevent backups.
- The northbound traffic will shift back into northbound lanes at the traffic light in front of the BJH emergency department.
- Traffic control flaggers will help keep vehicles moving.
Mid-April wrap up
Contractors will complete the utility work over a weekend in mid-April which will NOT require a lane shift or detour; however, northbound Kingshighway adjacent to the patient care tower will be reduced to one or two lanes starting at 8 p.m. Friday and concluding by 6 a.m. Monday. The dates will be communicated when finalized.
Alternate routes for team members and physicians
This work is expected to cause delays, especially on northbound Kingshighway. To avoid delays, team members and physicians who take Kingshighway have alternatives that provide easy access to all parking garages and lots, including the Plaza and Laclede garages:
- From Hwy. 40/I64: the Boyle and Tower Grove Ave. exits
- From I44: the Vandeventer exit or Kingshighway to Manchester to Taylor

IT Spotlight: Security Tips for Spring Break
Spring Break is right around the corner, and many in the WashU community will be traveling for conferences, studying away, researching elsewhere, visiting family, or just going somewhere relaxing. No matter where you go, your smartphone will undoubtedly be at your side. These handy devices have become our constant companions for just about anything you can think of, including making payments, storing boarding passes, producing maps of anywhere, finding rides, ordering food, and just about anything else you can imagine. Unfortunately, the devices we rely on for all these things have also become targets for theft and cybercrime.
Whether you’re going home or traveling for the break, please protect yourself and the WashU community. Remember the following travel tips to stay safe:
Travel Light
- Lighten your load and keep your belongings close to minimize the chance that something will be lost or stolen.
- Make a copy of your important documents. If you lose the originals, you can report loss or theft with the information on the copies. Contact your nearest U.S. embassy or consulate if you lost your passport outside the U.S.
- Minimize how much cash you carry. A cashless wallet is less valuable to a thief, and you can dispute credit card charges with the credit card company. If you are traveling, notify your credit card company so they don’t mistake your out-of-country purchases for fraudulent transactions.
- If you travel with a device, offload sensitive data before leaving. Save your files in WUSTLBox or OneDrive before leaving, and remove them from your device. Remember to check your Downloads folder and Trash for files containing sensitive and protected information.
- If you’re a faculty or staff member traveling for university business, consider using a loaner laptop for travel. These devices are encrypted to reduce the risk of unauthorized access to private or proprietary information.
When Using Public Wi-Fi
In the past, if you connected to a public Wi-Fi network, your information was at risk. Most websites didn’t use encryption to protect it from hackers snooping on the network.
Today, most websites encrypt your traffic, so connecting through a public Wi-Fi network is usually safe.
To know if your connection is encrypted, look for a lock symbol or https in the address bar to the left of the website address. This works on a mobile browser, too. It can be hard to tell if a mobile app uses encryption, but the majority do.
Smartphone Theft
- Do not let strangers use your smartphone.
- Set the lock screen to use passcode or biometric authentication.
- Share your location with emergency contacts on iPhone or Android. If you lose your phone, they can help locate it.
- Enable Find My Device on Apple and Android devices.
- Turn on Stolen Device Protection for iPhones to prevent someone from making changes to settings that can lock you out of your iPhone or Apple ID account. These measures help protect your device and account and give you more time to turn on Lost Mode using the Find My app or Find Devices on iCloud.com.
Register Your Trip
- If you’re traveling for university business, be sure to register on MyTrips International Travel Registry. Doing so will allow the university to help you in case of a problem or emergency. Registration is required for faculty and staff requesting a loaner laptop.
- Share your itinerary with someone you trust back home.
- Add luggage tags with your contact information in case they get lost.
- U.S. citizens and nationals traveling abroad should register with the Department of State’s Smart Traveler Enrollment Program (STEP). Also, be sure to check the Department of State website for travel advisories and information about how your devices may be screened during a border control check.
If your device is lost, stolen, or compromised during travel, contact the Office of Information Security at infosec@wustl.edu
Best wishes for a secure Spring Break!
| Keep up to date with IT news at the Office of Information Security blog |
Follow the Cardiovascular Division on X!
Check out our division account, @WashUCardiology! We will be sharing division accomplishments, announcements, news, events, and more. If you have a story about the cardiovascular division that you think deserves a social media spotlight, email bolhafner@wustl.edu.