ACE @ Wash U

In case you missed it…
In the webinar above, listen to presentations by amyloid specialists on treatments for neuropathic and cardiac amyloid. Dr. Mitchell discusses clinical trials and treating cardiovascular symptoms in cardic amyloid at the 23 minute and the 1 hour marks on the linked video above. Patient questions are asked and answered at the 1 hr and 20 minute mark.
What is amyloidosis?
Amyloidosis is a group of diseases caused by abnormal proteins that can affect multiple organ systems throughout the body. Depending on the type of protein, amyloid can lead to problems including stiffening of the heart and heart dysfunction, kidney disease, neuropathy, and issues with the digestive tract. These diseases require an integrated approach to diagnosis and treatment across multiple medical specialties.
Our Amyloid Center of Excellence (ACE) team includes experts in medical specialties including Cardiology, Hematology/Oncology, Neurology, Nephrology, Gastroenterology, Hepatology, Pulmonology and Pathology to ensure that each patient gets the correct diagnosis and receives the treatment that they need.
Providers or patients can contact the Amyloid Center of Excellence at Washington University/Barnes-Jewish Hospital (ACE@WashU) to obtain an appropriate evaluation and management plan for any amyloid type. The initial contact for the ACE team will usually be the hematology/oncology team at 314-454-8339 (especially for AL amyloid patients) or 314-362-1291 for the cardiology team (especially for patients with amyloid involvement of their heart). Either team can further direct the referral to other specialties.
Patients are welcome to call the above numbers directly to self-refer or make an appointment.
Referring physicians are welcome to contact us to speak directly to one of our physicians or to make a patient referral to the ACE @ Wash U.
Co-Directors
Bone Marrow Transplant (Hematology/Oncology)
Cardiology
Cardiac Imaging
Gastroenterology
Nephrology
Neurology
Pulmonology

Washington University is participating in the DepleTTR-CM study, and completed enrollment in May 2025 as the top enrolling site in the nation for this study. DepleTTR-CM is a fascinating new study that is investigating the ability of an antibody to remove amyloid from the body for patients with ATTR cardiomyopathy. Phase 1 data showed marked improvement in lab markers and imaging findings of amyloid. In this Phase III study, patients are enrolled 2:1 to ALXN2220 (study treatment) vs placebo.
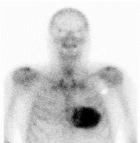
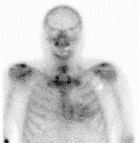
Regression of amyloid at 4 months on treatment with ALXN2220.
Washington University will begin enrollment in three trials in 2025 – CleopaTTRa, Magnitude and Triton.
In CleopaTTRa, we will be investigating the suspected benefit of another antibody, PRX004 (https://pubmed.ncbi.nlm.nih.gov/39472768/), to remove amyloid from the body similar to DepleTTR.
In Magnitude, we will be investigating the ability of CRISPR technology to edit the TTR gene to decrease TTR production by 80-90% indefinitely (https://www.nejm.org/doi/full/10.1056/NEJMoa2107454). This technology has been now studied for over 10 years and used successfully and safely in over 300 patients!
In Triton, we will investigate the ability of a new TTR silencer (nucresiran administered every 6 months) to improve amyloid outcomes in patients already on a stabilizer (tafamidis or acoramidis).
Amyloidosis is caused when abnormal proteins deposit in various organs including the heart, kidneys, lungs, liver, digestive tract, nerves and muscles.
There are over 30 different types of amyloid proteins, and it is essential to confirm the diagnosis of amyloid and the specific subtype to determine the optimal treatment approach.
Most amyloidosis is caused by one of two types:
AL (Light Chain) Amyloidosis is caused by a disorder of bone marrow cells (plasma cells) that is associated with multiple myeloma. AL amyloidosis is primarily treated by our hematology/oncology team while other specialists help with the care of any involved organs.
Transthryretin Amyloidosis (ATTR) is related to an overproduction of the TTR (Transports Thyroxine and Retinol) protein produced by the liver. ATTR can be a hereditary condition, and family members often need to be screened to ensure they do not share the responsible gene. ATTR is primarily treated by our cardiology or neurology specialists (or both) depending on whether it is predominantly causing heart or nerve issues.
Patients with amyloidosis can have a variety of symptoms which are based on the organ systems that have developed amyloid deposits. Symptoms are generally nonspecific and can include:
- Constipation or Diarrhea
- Weight Loss or Weight Gain
- Leg or Arm pain
- Peripheral Neuropathy
- Lower extremity weakness
- Carpal Tunnel Syndrome – pain in the wrists
- Shortness of breath with activity
- Leg or Arm lower swelling
- Lightheadedness, dizziness or fainting
- Generalized swelling in the abdomen, arms, legs
- Enlarged tongue
- Weakened voice
- Foamy urine
- Persistent nausea and vomiting
The diagnosis of amyloidosis is made by a combination of tests depending on a patient’s symptoms. Testing can include blood and urine tests as well as special imaging techniques.
Laboratory Testing may include:
- Complete blood count
- Blood measurements of kidney and liver function along with evaluation of blood proteins
- Blood clotting tests
- Blood cardiac biomarkers
- 24-hour urine collection to measure protein
- Genetic blood testing for genetic mutations (TTR amyloid)
Diagnostic Testing may include:
- Cardiac echocardiogram
- Cardiac MRI
- Body MRI
- Plain X-rays of the bones (skeletal survey)
- PET scans
- Technetium pyrophosphate scan (PYP scan)
- Measurement of nerve and muscle function (EMG)
The diagnosis of amyloidosis requires confirming amyloid deposition in tissues/organs with either a PYP scan or a biopsy. A PYP scan is similar to a CT scan but also uses a special molecule or tracer that makes amyloid light up in the heart. It cannot tell the difference between TTR and AL amyloid so it can only be used when the bloodwork is normal and there is no concern for AL amyloid.
Many patients will need a biopsy to confirm the diagnosis. The specific biopsies that may be performed will vary among patients depending on the organs that appear to be involved and the subtype of amyloid. Amyloid is detected by performing a special stain on the tissue biopsy called a Congo red stain. Special testing of liver and heart biopsies can include immune florescence staining and electron micrography. The tissue sample is then sent to a specialized lab to perform mass spectrometry to determine the amyloid subtype.
Biopsy sites may include:
- Bone marrow
- Heart
- Kidney
- Liver
- Nerve
- Muscle
- Gastrointestinal tract
- Skin
What To Expect On Your Initial Visit
The complete workup needed for amyloidosis can require comprehensive testing and involve physicians in different specialties in order to make the diagnosis, determine the amyloid type, and assess which organs are involved and to what degree.
Your initial visit to the Amyloid Center of Excellence at Washington University will involve a visit with one or more physicians. Multiple appointments over a few days may be required to complete the testing and to be evaluated by any needed physician groups.
For our patients traveling from far distances our team can help coordinate local accommodations for your stay in our area.
Hematology/Oncology/BMT
The BMT team is the first call for patients at risk for or diagnosed with AL amyloid, and can be reached at 314-454-8339
Cardiology
The Cardiology team can provide evaluations for any type of amyloid, especially when there is a concern for heart involvement of the amyloid.
Call cardiology at 314-362-1291
Gastroenterology
For patient with known amyloid and gastrointestinal (GI) symptoms, appointments with Dr. Blaney can be made directly at 314-454-8166
Neurology
For patients with neuropathy and diagnosed amyloid, or with concern for amyloid, you can contact our Neurology team for evaluation or management at 314-362-6981