Heart Matters – April/May 2024
Evolution of Heart-Valve Repair
From Curiosis Magazine
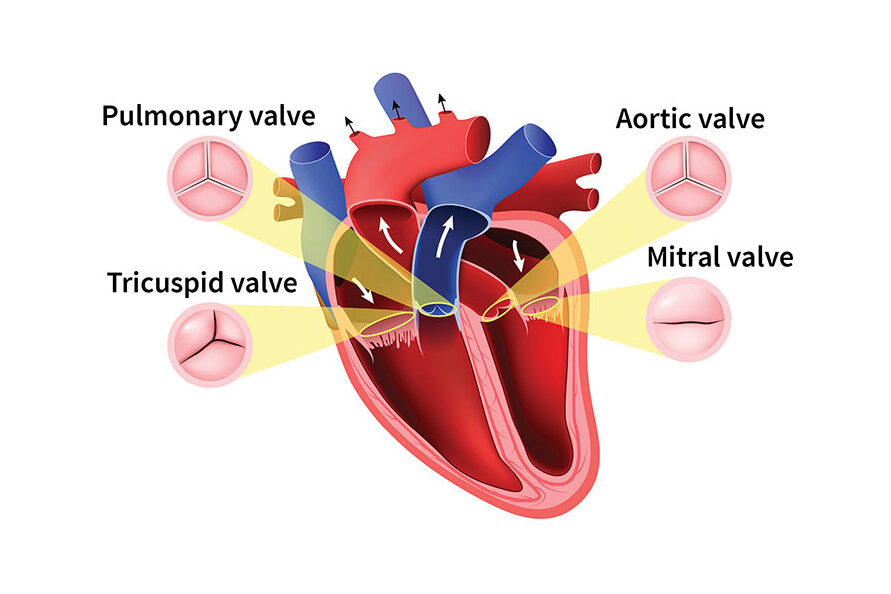
Study the anatomy of a human heart, and you’ll notice that there are four chambers and four valves that work sequentially to move blood into the heart and then out into the body. As the heart contracts and relaxes, its valves work in a set order, opening and closing to ensure that blood flows in one direction. One valve opens to allow blood to flow in and then closes to prevent backward flow.
When one or more valves are not working properly, resulting blood-flow problems may affect the heart and the rest of the body. While symptoms may be nonexistent or minor for years, malfunctioning valves can cause chest pain, shortness of breath, dizziness, fainting and swelling in the abdomen, ankles and feet. Upon examination, a physician may hear a “whoosh” sound or heart murmur and may detect abnormally low or high blood pressure, depending upon the valve affected. Some people with heart-valve problems notice an irregular heartbeat.
VALVE DISORDERS AND DISEASES

The four valves in the heart are called the aortic, mitral, pulmonary and tricuspid valves. The mitral valve has two flaps, called leaflets, that open and close; the others have three flaps. In broad categories, valve problems can be caused by:
- Stenosis: valve flaps become stiff or thick, preventing the valve from opening fully
- Regurgitation: valve flaps don’t close properly, causing blood to leak backwards
- Congenital abnormalities (present at birth)
The risk of developing heart-valve problems increases with age. Other risk factors include high blood pressure, high cholesterol, diabetes, obesity and a history of coronary artery disease and heart failure. Infections, particularly rheumatic fever, also can damage heart valves.
Left untreated, heart-valve disorders can lead to strokes, blood clots, heart rhythm problems, even heart failure. Advances made in cardiology and heart surgery now allow specialists to repair or replace any of the four heart valves using a variety of techniques, including minimally invasive surgery.
VALVE REPAIR: A SHORT HISTORY
The first successful mitral valve repair was documented in 1923 at Brigham and Women’s Hospital in Boston. It wasn’t until the development of the heart-lung bypass machine in 1953, however, that open heart surgery made it possible to treat valve disease effectively.
The first artificial mechanical heart valve was developed in 1952 by Charles Hufnagel, MD, a surgeon at Georgetown University. Called a ball and cage valve, it functioned like a marble in a tube. When the heart contracted, the resulting pressure caused the ball to rise to a wider section of the tube, enabling blood to flow through. Once the muscle relaxed, the ball dropped, and the opening closed. The first mechanical mitral valve replacement took place in 1960; replacement with a mechanical aortic valve occurred just a year later. Within the same decade, donor grafts became an option, with valve tissue harvested from a deceased human donor (called an allograft) or from a pig or cow (called a xenograft).
In the late 1960s, a new procedure came to the forefront to treat aortic valve disease. Called the Ross procedure, it was developed by London heart surgeon Donald Ross, MD. During this treatment, the surgeon removes the non-functioning aortic valve from the patient, replacing it with the patient’s own pulmonary valve. A donor pulmonary valve is then implanted to replace the one that has been moved.
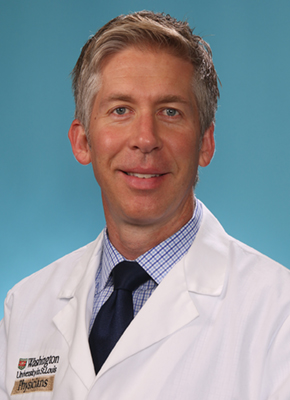
Tsuyoshi Kaneko, MD, Washington University cardiothoracic surgeon at Barnes-Jewish Hospital and chief of the university’s section of cardiac surgery, explains that a pulmonary valve is like an aortic valve in size and shape. The Ross procedure is effective because it substitutes the failing aortic valve with the patient’s own pulmonary valve, which can manage the job of an aortic valve with less risk of failure than other replacement options. Because the donor valve implanted into the pulmonary position is under less stress than it would be in the aortic position, it is more likely to function long-term.
“This procedure can be effective in treating severe aortic valve disease in both children and adults,” Kaneko says. “And, unlike standard surgical aortic valve replacement or even less invasive procedures, the Ross procedure remains the only treatment option that restores normal life expectancy to young and middle-aged patients with aortic stenosis.” For patients in this age group who are treated with the Ross procedure, Kaneko says, “fewer than a third require further intervention up to 25 years after the initial surgery.”
ADVANCING THE FIELD
While open-heart surgery is often used to treat valve disease in people under 60, less invasive, transcatheter procedures are becoming more common. Offering excellent outcomes and faster recovery times for patients, this treatment uses a small catheter that is threaded into an artery through a small incision in the groin or chest. The surgeon moves the catheter through the artery to the diseased valve, where it is used to remove the valve and replace it with a new one.
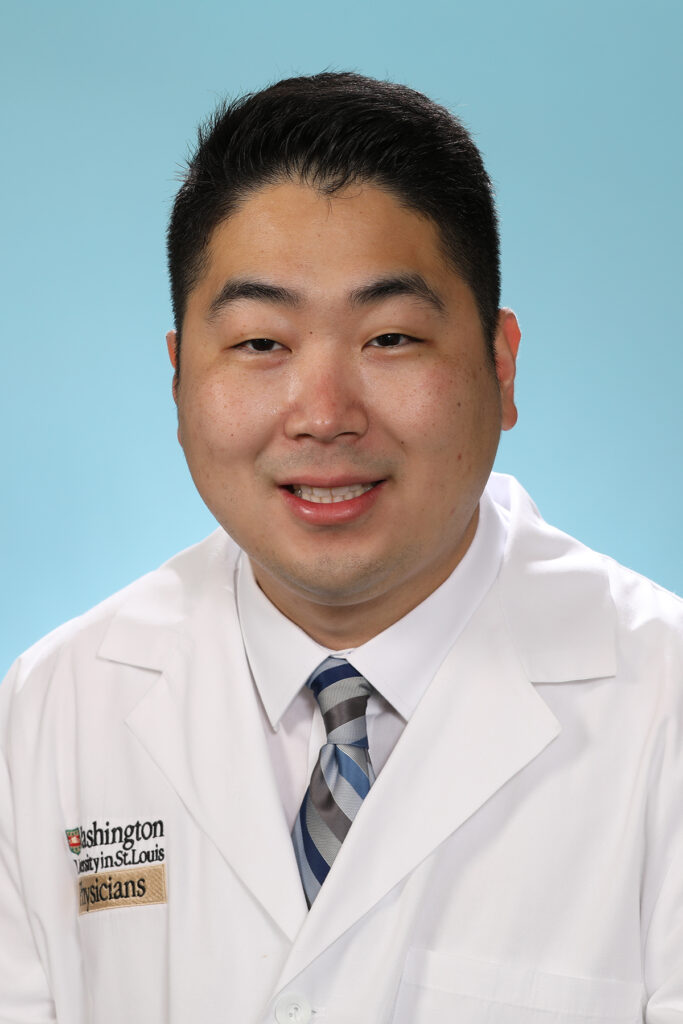
Specialists at the Washington University and Barnes-Jewish Heart & Vascular Center have pioneered several types of minimally invasive valve surgeries. Alan Zajarias, MD, interventional cardiologist at the center, performed St. Louis’ first transcatheter aortic valve replacement, also known as TAVR, in 2008, working with cardiothoracic surgeon Ralph Damiano, MD, and interventional cardiologist John Lasala, MD, PhD. The U.S. Food & Drug Administration (FDA) formally approved the TAVR procedure for aortic valve replacement in 2010. Two years later, specialists in Denmark performed the first human transcatheter mitral valve replacement procedure.
In 2021, the Heart & Vascular Center’s valve team was among the first in the world to use a transfemoral approach, through an artery in the leg, in a procedure to treat severe regurgitation in a tricuspid valve. “It was during the COVID-19 pandemic, and we received special, ‘compassionate care’ approval from the FDA to use a mitral valve device to treat tricuspid regurgitation in a patient who had failed three previous bypass surgeries,” says Zajarias, who performed the procedure with cardiovascular surgeon Puja Kachroo, MD, and other colleagues. “It worked beautifully.”
Transcatheter tricuspid valve replacement is now an evolving advancement in valve replacement techniques.
VALVE REPLACEMENT OPTIONS
The two types of replacement valves available— mechanical and natural tissue—present two different sets of factors to consider. Mechanical devices require that patients take blood-thinning medications for the rest of their lives. Biologic tissue valves do not require blood thinners; however, they wear out and often need replacement within 10 to 20 years. Both Kaneko and Zajarias note that newer TAVR devices are smaller and more sophisticated, and their delivery systems—the way these devices are deployed in the body—are improving. As a result, specialists can now access the valve through smaller femoral blood vessels and more accurately position replacement valves for optimal outcomes.
“TAVR is a good, safe procedure for patients with aortic stenosis,” Zajarias says. “In older patients, it is often the procedure of choice. For younger patients, we have a thoughtful conversation concerning the risks and benefits of each valve type, taking into consideration their own anatomy and other health concerns, in addition to age.”
According to the Centers for Disease Control and Prevention:
2.5% of the U.S. population have valvular heart disease, most notably in the older adult population
25,000 estimated deaths in the United States each year are attributed to valvular heart disease
“The concept of lifetime management has become a new conversation in our field,” Kaneko says. “As we perform heart-valve procedures on younger people—those in their 50s or 60s—we know that there is a strong predictability they will need another procedure in their 80s because many replacement heart valves wear out over time.” Both Zajarias and Kaneko note that ongoing research and clinical trials are working to identify better valve designs and materials that will offer more options to patients.
ARTIFICIAL INTELLIGENCE AND HEART-VALVE TREATMENT
Artificial intelligence (AI) and computer simulation tools have opened up new possibilities in the treatment of valve disease. These technologies are being used to aid in planning before surgery and in optimizing long-term use of replacement valves.
In planning valve surgery, Zajarias says, “there’s a lot of consideration given to which replacement valve should be used and how it should be placed. New technology allows us to simulate placement to determine the best option. AI tools also provide a computer simulation of what might happen if or when we must do another procedure farther down the line to replace that valve again.”
As more data becomes available that can inform artificial intelligence tools, Kaneko and Zajarias point out, the technology has the potential to produce even more accurate predictive modeling. And they anticipate it will become a critical element in treating heart-valve disease in younger patients, an important consideration given that valvular disease is on the rise around the globe.
“What we do today for patients will affect their overall health and health-care decisions years down the road,” Zajarias says. “AI and computer simulations help us make better decisions about the first interventions we undertake for patients, and they can help us better predict how they will do long-term. In effect, we now have better, more accurate ways to care for people with valvular heart disease.”
Braverman Hosts 15th Heartworks Gala Benefiting Marfan Foundation

“What started as an idea 16 years ago has led to one of the most impactful fundraisers supporting The Marfan Foundation.”
In a joint statement, husband and wife co-founders of the St. Louis Heartworks Gala, Dr. Alan Braverman and Mrs. Rebecca Braverman, took a moment to reflect on the event’s 15th anniversary. Heartworks was held at The Four Seasons on April 27th. The Bravermans said Heartworks is meaningful to them for so many reasons.
“Our gala provides awareness of the incredible work of The Marfan Foundation and raises important funds for the Foundation’s programs that improve the lives of people with genetic aortic conditions. The gala brings together our loyal supporters that include a community of friends, colleagues, and affected individuals and their families for an evening of celebration,” said the Bravermans.
Dr. Sanjeev Bhalla, MD a professor of radiology at the Mallinckrodt Institute of Radiology (MIR) within Washington University School of Medicine, and Hero with a Heart honoree last year, described the impact of the Heartworks gala for him.
“For over 20 years, I have dedicated my career to the radiology of the aorta and aortic conditions. The Heartworks St. Louis Gala is a great opportunity to bring together the whole community of people who want to make a difference in the care of patients with aortic and vascular conditions,” said Bhalla.
For Alan Braverman, highlighting the impactful work of The Marfan Foundation to support community members living with Marfan and related conditions is primary.
“While we honor heroes in medicine, research, volunteerism and philanthropy in a heartfelt and meaningful event, the funds raised at our Gala directly support the many critical functions of The Foundations in education, research, and awareness.”
This year, two physicians were honored: Dr. John Westley “Wes” Ohman and Dr. Luis A. Sanchez, both for their outstanding work in treating patients living with genetic aortic and vascular conditions.
Dr. Ohman is Associate Professor and Program Director for the Integrated Vascular Surgery Residency in the Section of Vascular Surgery at Washington University School of Medicine. He’s a member of the Society for Vascular Surgery, Midwestern Vascular Surgery, and Vascular and Endovascular Surgery Society. His research interests include treatment of complex aortic diseases, surgical care, and behavior of the thoracoabdominal aorta after aortic dissection in individuals with genetically triggered aortic syndromes like Marfan, Loeys-Dietz, and VEDS. Dr. Ohman’s clinical interests likewise include treating people with genetic aortic and vascular conditions surgically.
Dr. Sanchez has been the Chief of the Section of Vascular Surgery since 2011 and Professor of Surgery and Radiology at Washington University School of Medicine since 2006. He has been Co-Director of the Barnes-Jewish Hospital Heart and Vascular Center since 2011 and the Chairman of the WUSM Conflict of interest Committee since 2021. Additionally, he is Vascular Surgery Director at BJH and Missouri Baptist Hospitals. Dr. Sanchez has been President of the International Society of Spanish Speaking Vascular Surgeons and in 2017 received the Dr. Mario Garcia Palmieri Global Education Award at the 8th NACET Interdisciplinary Summit.
In addition to building and celebrating community, the gala aims to save and improve lives by raising $350K to benefit the Foundation’s research, education, and support initiatives. While the gala has a long-standing history, new supporters enhance the impact of the event every year.
“For first-time attendees, we welcome you into The Marfan Foundation family and appreciate your interest in this most impactful organization dedicated to improving the lives of affected individuals and their families,” said the Bravermans.
Dr. Bhalla summarized the feeling the event leaves with supporters who attend, “You go into the dinner thinking you are making a change and when you leave, you realize you have been changed by the kindness and compassion of the patients, their families, the physicians and scientists working with the foundation,” said Bhalla.
About 1 in 5,000 people have Marfan syndrome, including men and women of all races and ethnic groups. Roughly 3 out of 4 people with Marfan syndrome inherit it. There is a 50 percent chance that a person with Marfan syndrome will pass along the genetic mutation each time they have a child. Because connective tissue is found throughout the body, Marfan syndrome can affect many different parts of the body. Features of the condition are most often found in the heart, blood vessels, bones, joints, and eyes. Some Marfan features – for example, aortic enlargement (expansion of the main blood vessel that carries blood away from the heart to the rest of the body) – can be life-threatening. The lungs, skin, and nervous system may also be affected.
About the Marfan Foundation
The Marfan Foundation is a nonprofit organization that empowers people living with genetic aortic and vascular conditions to foster optimal quality of life and longevity. We save lives through research and education that enables healthcare providers to offer best-quality treatment. We serve communities impacted by Marfan syndrome, Loeys-Dietz syndrome, Vascular Ehlers-Danlos Syndrome and related conditions. To learn more, visit marfan.org
ACC Updates HFrEF Decision Pathway, Reinforcing the Four Pillars of Therapy
The document also strengthens advice regarding which medications should be started in all patients
Thomas M. Maddox, MD, MSc, Professor of Medicine in the Cardiovascular Division at WashU Medicine, and colleagues recently published an Expert Consensus Decision Pathway (ECDP) for the many decisions required in the management and treatment of patients with heart failure with reduced ejection fraction (HFrEF). The document was published in the Journal of the American College of Cardiology.
“This decision pathway, updated with the latest evidence for HFrEF management, is an essential contribution to every clinician’s toolbox,” says Maddox. “It contains clear and simple HFrEF management pathways and practical advice in managing these complex patients.”Thomas Maddox, MD
Specifically, the ECDP provides updated guidance on 10 pivotal issues in HFrEF, including how to initiate, add or switch therapies with consideration of newer evidence-based guideline-directed treatments for HFrEF. It also addresses how to achieve optimal therapy given multiple drugs for HF, including augmented clinical assessment that may trigger modifications in guideline-directed therapy. Additionally, the ECDP provides guidance for managing the increasing complexity of heart failure, as well as common comorbidities.
Artificial Intelligence for Cardiovascular Care
Thomas M. Maddox, MD, MSc, Professor of Medicine, Cardiovascular Division at WashU Medicine, and colleagues recently published two articles outlining the current opportunities for AI to impact cardiovascular care.
The articles are published in the Journal of the American College of Cardiology:
- Artificial Intelligence for Cardiovascular Care – Part 1: Advances: JACC Review Topic of the Week
- Artificial Intelligence in Cardiovascular Care – Part 2: Applications: JACC Review Topic of the Week
These articles highlight how AI is poised to affect almost every aspect of cardiovascular care. ” says Maddox. “Our group hopes that this work helps prepare clinicians for what’s to come”.
Specifically, the review articles highlight how AI in cardiovascular care enhances diagnosis and treatment, improving outcomes through better measurements, image quality, and disease detection. The articles also highlight the need for comprehensive validation of AI’s application in clinical care, recognizing that definitive evidence of AI’s impact on patient outcomes is pending, with trials of the technology underway. Adopting these technologies responsibly, with high standards for efficacy, is vital for their future role in cardiology.
Fellow Kyle Yoo on World Heart Federation Podcast
Cardiovascular Fellow Kyle Yoo appeared on the second episode of new podcast series ‘Global Heart Podcast’, with World Heart Federation Science Advisor Pablo Perel and Global Heart Journal Editor-in-chief Rick Grobbee. The episode focused on discussions of recent global cardiovascular research on secondary prevention and explaining findings and implications with lead authors of the papers.
Dr. Yoo discussed his recent work Aspirin for Secondary Prevention of Cardiovascular Disease in 51 Low-, Middle-, and High-Income Countries.
Listen to the episode here
Thakker Coauthors Research Letter in JACC
Dr. Prashanth Thakker, Assistant Professor of Medicine and Associate Director of Program Development in the Cardiovascular Fellowship program was coauthor of a research letter published in the Journal of the American College of Cardiology titled “A Leadership Program to Support Career Development of Cardiovascular Chief Fellows”.
The letter details the importance of the role of chief fellow within a fellowship program, and explored ways to support the development of individuals in training programs in this role.
View full article here
Stitziel Elected to the Association of University Cardiologists

Professor of Medicine Nathan Stitziel, MD, PhD was recently elected to the prestigious Association of University Cardiologists. Active membership in the United States is limited to just 135 cardiologists “who shape the course of research and training in cardiovascular disease.”
From the AUC website:
Founded in 1961, the Association of University Cardiologists (AUC) is an organization that is limited to an active membership of 135 academic cardiologists from the United States, elected by their peers.
The group has a purely educational purpose and meets once per year in January for a two-day session of scientific interchange. The members traditionally are the leaders and best investigators in American cardiology.
The Association of University Cardiologists contains those cardiologists who shape the course of research and training in cardiovascular disease in this country.
Congratulations to Dr. Stitziel on this accomplishment!

Quader Elected to ASE Board of Directors
Associate Professor of Medicine Nishath Quader, MD, has been elected to the board of the American Society of Echocardiographers, to serve a term that will begin in July 2024.
The American Society of Echocardiography is an organization of professionals working to advance cardiovascular ultrasound and improve lives through excellence in education, research, innovation, advocacy, and service to the profession and the public.
Congratulations to Dr. Quader on this honor!
Huffman Named William Bowen Endowed Professor

Mark D. Huffman, MD, MPH, tenured Professor of Medicine and Co-Director of the DOM Global Health Center, has been appointed as the inaugural William Bowen Endowed Professor. The appointment recognizes Dr. Huffman’s outstanding leadership in preventive cardiology and cardiovascular health research at an individual and population level, and at a global scale. His research program seeks to improve global cardiovascular health and health care across the spectrum of disease prevention, and implement evidence-based interventions into routine practice and policy.
Some of his major scientific contributions that have affected practice and policy include: 1) developing and testing new combination therapies for the treatment of high blood pressure in federally qualified health centers in Chicago and for the treatment of heart failure in South Asia; 2) leading the largest cardiovascular randomized trial conducted in India to improve the quality of heart attack care in the south Indian state of Kerala in collaboration with the Centre for Chronic Disease Control and Cardiological Society of India; 3) leading one of the largest and most successful hypertension control programs in Africa in collaboration with University of Abuja; 4) synthesizing the effects of evidence-based interventions to inform clinical practice guidelines and global health policy, ranging from surgical strategies to treat atrial fibrillation for the European Society of Cardiology for the 2016 European guidelines to polypills for the prevention of heart attacks and strokes, which were added to the World Health Organization’s Model List of Essential Medicines in 2023; 5) estimating the long-term, or lifetime, risks for heart failure in diverse populations in the United States; and 6) synthesizing evidence on polypills for global cardiovascular disease prevention and control.
Congratulations on this achievement and recognition!

Thakker Named Program Director for the Cardiovascular Disease Fellowship
Effective April 1,2024, Dr. Prashanth Thakker has been appointed as the new Program Director for the Cardiovascular Disease Fellowship, succeeding Dr. Andy Kates who has served admirably in this role for the last 16 years.
Dr. Thakker received his MD from Northeast Ohio Medical University in 2013 as part of the BS/MD program with the University of Akron. He then completed internal medicine residency and a Chief resident year at Case Western University. In 2017, he joined the Wash U General Cardiology Fellowship training program, serving as Chief Fellow for two years, and then completed his Interventional Fellowship. He joined the Washington University Cardiovascular Division as Assistant Professor in 2021 and served as Associate Program Director for Program Development prior to his new appointment.
Dr. Thakker brings a wealth of experience in medical education as the next Fellowship Program Director. He obtained a Master’s Degree in Health Professions Education during his fellowship training and also completed the Foundations in Teaching Skills Program. He also served as Assistant Program Director of the Washington University Teaching Physicians Pathway. As Associate Program Director, Prashanth helped to revise and revamp the educational curriculum for the fellowship program. He was recognized with the Saligman-Reiss Award for Excellence in Teaching in 2022.
Dr. Andy Kates has served as the Fellowship Program Director since 2008. During that time, he oversaw the robust growth and development of the program to the elite, uniquely designed and diverse fellowship dedicated to mentorship that it is today. In his capacity as the program director, Dr. Kates has directly trained more than 140 cardiology fellows, many of whom have developed into leaders across the spectrum of cardiovascular medicine, across the region, the US, and the world.
Dr. Kates will remain in his position as Associate Chief for Education and will continue to lead the educational mission of the Division. During the leadership transition period, he will also remain with the fellowship program as an Associate Program Director to provide support and mentorship. In addition, he will assist in developing other clinical areas within the division related to general cardiology.
Brown Among Partnership Development and Sustainability Support Program (PDSS) 2024-2025 Awardees

Dr. Angela Brown, Professor of Medicine in the Cardiovascular Division, is among this year’s awardees for the Partnership Development and Sustainability Support Program with the Washington University School of Medicine ICTS.
Her proposal, Community Wholeness in Fountain Park: Creating a Meaningful Research Agenda for Health Equity is described below:
Summary: A partnership between Centennial Christian Church and the Our Community Our Health (OCOH) team began as a COVID-19 response. OCOH maintains a recurring schedule and “pops up” a mobile vaccine clinic alongside food ministry services. The work has been driven by aligning university resources with community priorities. In the next phase of this partnership, we will: 1) identify and rank community priorities surrounding social determinants of health; 2) set partnership recommendations; and 3) create a meaningful action agenda grounded in community-based participatory research and human-centered design to advance health equity in Fountain Park.
Partnership Development and Sustainability Support Program (PDSS) 2024-2025 Awardees

Sadhu Selected as DASP Faculty Honoree
Associate Professor of Medicine Dr. Justin Sadhu is a 2023-2024 faculty honoree of the Washington University Distinguished ALumni Scholarship Program.
Created in 1989, the Distinguished Alumni Scholarship Program (DASP) grants four entering students per year a four-year, full-tuition scholarship, for a total of 16 DASP students at the school at one time. Institutional funds are blended with annual support to the Medical Teaching Fund to make these scholarships possible.
The Washington University Medical Center Alumni Association (WUMCAA) Executive Council is connected to DASP through both the funding of the scholarships and the honoring of alumni. Each year, the Executive Council selects four outstanding alumni to honor as namesakes of these scholarships. Each student’s scholarship bears the name of an alumnus or alumna who has served on the School of Medicine faculty, past or present, with particular distinction.
A faculty committee selects the students based on exceptional academic achievement and character. Students who continue to meet eligibility requirements will hold the scholarships until they graduate.
Each fall, the new student scholarship recipients and alumni honorees gather at a luncheon where the students have the opportunity to meet the outstanding alumni for whom their scholarships are named.
Keep up to date with all Division news on our news page!
Way to Shine!
“I worked with Tara Ward today. (She showed up to clinic and attended with me. Given that I did not even request she do this, I was incredibly impressed!) Additionally, she was amazing with the patient and made huge efforts to start to understand the work flow.”
Other Way to Shine’s for March and April were Barb Stehman, Dana Gima, Ann Mahoney, Kinsey Walker, Angie Smith, Holley Crabtree, Morgan Porter, Lisa Murphy, Anne Buechler, Becky Prsha, Donna Fuehne, Katherine Ramsay, Megan Hangyal, Deana Wilmesher, Anne Yoggerst, Lauren LaRose, Gina Bliss-Braymer, Ryan Gilliam, Karen Moore, Katie Fenwick, Tori Menning, Karen Moore, Sharon Sauer, Brittney Turner, Jill Taake, Jennifer Lyerla, Millie Cova, Allison Schremp, Emma Porter, Mandy Harris, Kelsey Fassold, Nicole Thompson, Jessica Wagner, Dr. Adam Lick, and Paige Rama!
If you catch someone in the act of shining, contact or send an email to bolhafner@wustl.edu.
Clinical Spotlight: LVAD Clinic

Each month, Heart Matters will highlight a research lab or clinical program. We want everyone in the division to be proud of the work we do across all of our locations and disciplines.
The Washington University Physicians LVAD clinic team offer life-saving care and support for patients who are waiting for or ineligible for a heart transplant.
A left ventricular assist device (LVAD) is implanted in the chest. It helps pump blood from the lower left heart chamber, called the left ventricle, to the rest of the body. A controller unit and battery pack are worn outside the body and are connected to the LVAD through a small opening in the skin.
Working out of the West County Heart and Vascular Center, the team is led by Drs. Ewald and Hartupee, and Nurse Practitioner Heidi Craddock. LVAD Nurse Coordinators include Lydia Hohenstein, Amanda Blackford, Denise Manker, and Nancy Ledee. Recently, Clinical Research Coordinator Chris Cross joined the clinic in conjunction with CT surgery. The clinic sees patients every Thursday, and has a total of 169 patients as of this writing.
The LVAD clinic originally started in the CAM in 1997. At that time, the program was much smaller, serving only around 25 patients. Heidi Craddock notes that it was ahead of its time for being largely nurse-run. Patients with an LVAD, as well as their families and caregivers, need a significant amount of specialized support, so it is important for them to have a dedicated team with the expertise to make sure they remain stable at home.
“Most of our patients”, says Heidi “begin their journey with a catastrophic hospital stay”, having heart failure that leads to a major cardiac emergency. If someone is in heart failure but ineligible for transplant, for instance due to a comorbidity such as smoking, LVAD can be the answer.
Dr. Hartupee explains, “LVAD gives patient with endstage heart failure another option. For some patients LVAD support is used as a bridge to transplant for those that are too ill to go directly to transplant. For others the plan is for them to remain on mechanical support for the rest of the life. Outcomes with respect to both survival and adverse events have continued to improve. LVAD not only offers increased survival, but patients can have a very good quality of life on LVAD support.”
The LVAD team gets very familiar with their patients. Nurse Lydia Hohenstein says that even though they have so many individual patients, “if you name one, we can tell you a lot of things about them”. They see patients every few weeks to every few months depending on how healthy they are and what their needs are at the time. They also provide ongoing education for the patients and caregivers about the specific needs of an LVAD user.
Nurse Amanda Blackford explains that the patients have to come in so often because of the details they collect at each visit. “They can’t use a normal blood pressure cuff”, says Amanda, “so we have to use a doppler”. Their device is connected to a screen which displays and collects various data, they have blood drawn and are checked for any sign of infection, and discuss how they have been doing since their last visit. Heidi, Dr. Hartupee, or Dr. Ewald will answer any medical questions and consult with the patients about transplant candidacy.
Patients also have the opportunity to combine their visit with other specialist visits the same day, which is convenient for them and reduces travel and confusion. “Many of the issues patients experience post LVAD are non cardiac and we work closely with other groups including GI and ID,” says Dr. Hartupee.
St. Louis is serving a large area without any other LVAD clinics, including much of Missouri and Illinois, as well as Arkansas and Oklahoma. Quarterly, some of the clinic staff travel to Joplin to see patients at the Freeman Heart & Vascular Institute, saving some of the farther flung patients hours of travel.
Lydia says that working with LVAD patients is rewarding because you can learn so much about such a specialized field, but also because they are giving the patients “another chance at life”. Heidi echoes this sentiment, noting that “Death sentences aren’t always death sentences anymore.”
The clinic was recently able to restart an in-person support group for LVAD patients. During the COVID pandemic, there were some attempts to host one remotely, but patients really wanted the human connection of meeting face-to-face. Now that it is safer to meet in-person, the support group numbers are growing again, and is just one more way this caring team is improving their patients’ lives.
21st Annual Scientific Sessions: Interorgan Crosstalk in Heart and Vascular Metabolism

Me In St. Louis
Welcome! We are pleased to invite you to the 21st Annual Meeting of the Society for Heart and Vascular Metabolism (SHVM), to be held in Saint Louis, Missouri, from Sunday, September 8th to Wednesday the 11th, 2024. In keeping with the 20-year tradition of SHVM meetings, this event will gather investigators from around the globe to provide a forum for the free exchange of ideas, to promote scientific interactions between young researchers and senior scientists in formal and informal settings, and to provide an atmosphere that fosters new collaborations.
Division Staffing Updates
Positions open for hiring:
JR72592 Research Cardiac Sonographer (PRN) – CORE Lab
JR77820 Clinical Specialist PT/OT (PRN) – Clinical Trials
JR80032 Clinical Research Coordinator I – Clinical Trials
JR80321 Research Opportunities – Dr. Prabhu’s Lab
JR78663 Research Opportunities – Dr. Rentschler Lab
JR80555 Staff Scientist – Sah Lab
JR78795 Postdoctoral Research Associate – Dr. Stitziel’s Lab
JR81508 Medical Secretary II
JR81763 Research Nurse Coordinator I
JR81766 Postdoc Res Assoc – Sah Lab
Welcome to the Cardiovascular Division:
Yuqian Xie – Res Tech I – Dr. Rentschler’s Lab – 3/1/2024
Jill Powles – Clinical Nurse Coordinator – VALVE TEAM – 3/1/2024
Brielle Stephens – Medical Assistant III – West County Practice – 3/25/2024
Kimberly Britton – Registered Medical Assistant III (South County) – 4/1/2024
Felicia Garcia-Allen – Clinical Nurse Coordinator – HCM Ctr – 4/8/2024
Marlana Blackmon – Registered Medical Assistant III – NWT – 4/8/2024
Caroline Chou – Clinical Research Coordinator I – Clinical Trials – 4/22/2024
Jay Restifo – Research Cardiac Sonographer – CORE LAB – 4/29/2024
Jamie Vaughn – Senior Department Accounting Assistant – PURCHASING TEAM – 4/29/2024
Farewell:
Farewell to these Cardiovascular Division employees. Thank you for your service, you will be missed!
Corriauna Harper – 3/11/2024
Cynthia Ousley – 4/5/2024
Antanisha Parks – 4/17/2024
Emily Titzler – 4/24/2024
Mary Wingate – 5/1/2024
Congratulations on your Retirement, Mary!
Beloved member of the Cardiovascular Division team, Mary Wingate has retired as of May 1st. The division held a party in Northwest Tower’s kitchen to recognize her long time contributions as Assistant to the Chief, and say a bittersweet goodbye.
We are pleased to announce that Nikki Padilla is joining the Cardiovascular Division to support Dr. Prabhu in the Assistant to the Chief role effective May 13th. Nikki comes to Washington University from the state of Colorado where she has worked in various healthcare administrative positions over the last 7 years.
To aid in this transition, Nikki Madigan has generously agreed to assist Dr. Prabhu after Mary Wingate’s departure and during Nikki Padilla’s onboarding period. Thank you again to Mary Wingate for her many years of service to the Cardiovascular Division!



Health and Wellness
Vitamin D: The Sunshine Vitamin
James Chilton, Dietetic Intern at Logan University,
Emma Greenhill, MS, RD, LDN
How Much Vitamin D is needed each day? Recommended daily intakes (RDAs) for Vitamin D include:
| Age | Male | Female | Pregnancy | Lactation |
| 0-12 months (AlI) | 10 mcg (400 IU) | 10 mcg (400IU) | ||
| 1-13 years | 15mcg (600 IU) | 15mcg (600 IU) | ||
| 12-18 years | 15mcg (600 IU) | 15mcg (600 IU) | 15mcg (600 IU) | 15mcg (600 IU) |
| 19-50 years | 15mcg (600 IU) | 15mcg (600 IU) | 15mcg (600 IU) | 15mcg (600 IU) |
| 51-70 years | 15mcg (600 IU) | 15mcg (600 IU) | ||
| >70 years | 20 mcg (800 IU) | 20 mcg (800 IU) |
How The Body Produces Vitamin D. Vitamin D is unique in that it is one of the few vitamins that our body can produce on its own in large amounts. Vitamin D is synthesized after exposure to ultraviolet B radiation from the sun which produces approximately 80% of total vitamin D in the body and may last longer than what is ingested from dietary sources. Sunlight activates precursors of vitamin D known as 7-dehydrocholesterol to form pre-vitamin D3 (cholecalciferol) which circulates through the blood stream to the liver and then kidneys to be converted into active form known as vitamin D 1,25(OH) 2D. Current research suggests that receiving 5 to 30 minutes of sun exposure, primarily between 10 am and 4 pm per day or at least twice per week may provide adequate amounts of vitamin D.
Dietary Sources of Vitamin D. While our body can produce a large portion of Vitamin D from sun exposure, obtaining vitamin D through diet is necessary to meet daily nutrient needs. Dietary sources of vitamin D are especially important for individuals who live in areas with limited sun exposure as well as individuals who spend a significant amount of time inside without sun exposure. Dietary sources rich in vitamin D include fatty fish like salmon, trout, tuna, mackerel, moderate amounts in animal sources such as egg yolks, beef liver, and cheese, as well as small amounts in mushrooms. In addition to these foods, vitamin D is found in fortified dairy products, plant-based milk alternatives, some juices, and some cereals.
Are Supplements Just as Good as Sun Exposure or Dietary Sources? Both forms of vitamin D Supplements (D2 and D3) can increase serum 25(OH)D levels as they share nearly identical metabolic pathways in the body; however, D3 may be more effective in maintaining serum 25 (OH)D levels when compared to D2. Since vitamin D is a fat-soluble vitamin, the presence of dietary fat may improve absorption in the gut. Therefore, choosing fatty fish and dairy products that may be fortified with vitamin D more often may support greater absorption. When taking a vitamin D dietary supplement, consider taking it with food to increase absorption. While dietary supplements may be helpful to meet RDAs for vitamin D, obtaining vitamin D from sun exposure and food sources to obtain other important vitamins and minerals is preferred.
Pretty in Pink Peach Smoothie

Serves: 1 • Prep Time: 5 mins • Total Time: 5 mins
Ingredients
For the smoothie:
- 1 cup frozen peach slices
- 1 cup frozen raspberries or strawberries
- ½ cup vanilla or plain greek yogurt
- 1 cup skim milk (or plant-based alternative)
- 1 teaspoon pure vanilla extract
To garnish:
- Granola
- Raspberries
- Peach slices
Directions
- Add all ingredients to a high-powered blender: frozen peaches, frozen raspberries, yogurt, milk and vanilla extract. Blend until smooth, adding more milk to thin, if necessary.
- Feel free to add any optional add-ins to your smoothie if you’d like.
- Pour into a glass and enjoy!
Tips
- Add all ingredients to a high-powered blender: frozen peaches, frozen raspberries, yogurt, milk and vanilla extract. Blend until smooth, adding more milk to thin, if necessary.
- Feel free to add any optional add-ins to your smoothie if you’d like.
- Pour into a glass and enjoy!
Reference
- Recipe from: https://www.ambitiouskitchen.com/peach-smoothie/
- Nair, R., & Maseeh, A. (2012). Vitamin D: The “sunshine” vitamin. Journal of pharmacology & pharmacotherapeutics, 3(2), 118–126. https://doi.org/10.4103/0976-500X.95506
- Office of dietary supplements (2023). Vitamin d. National Institutes of Health. https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/ Raymond-Lezman, J. R., & Riskin, S. I. (2023). Benefits and risks of sun exposure to maintain adequate vitamin D levels. Curēus. https://doi.org/10.7759/cureus.38578
Do you have BJC Cigna? Remember that you have annual coverage to meet with me, Emma Greenhill, a Heart Care Institute dietitian. Call 314-996-8165 for more insurance information or to schedule an appointment.
DOM Success Spotlights
The Department of Medicine marketing team has created a new way for you to share with us about your achievements, publications, research, and educational opportunities. We now have a Success Spotlight page on our Department of Medicine website. This page will allow you to quickly enter in pertinent information regarding your success. Be it a leadership role, publication, new research, clinical work, educational opportunities, news media interviews and more.
The marketing team will reach out to you to gather any additional information they may need to help amplify your project. We hope you’ll take the opportunity to use this feature so we can do our part in supporting your successes! Our goal is to help streamline the method for sharing this information so that we can disseminate the information across DOM, WashU Medicine and all our social channels. Sharing your achievements will help make the St. Louis community, as well as those around the world, aware the amazing things happening here at WashU Department of Medicine.
WashU Night at the Ballpark

Join your colleagues, friends and family for WashU’s Night at the Ballpark on Sept. 6, 2024! The St. Louis Cardinals will take on the Seattle Mariners and the first pitch will be thrown out at 7:15 p.m. CT.
View the Busch Stadium Cardinals Seating Guide. Ticket sales will end on Aug. 9, 2024, at 12 p.m. CT.
Tickets are available on a first-come-first-serve basis and must be purchased via credit/debit card. For larger groups, all tickets should be purchased in one transaction to ensure you’re seated together. This year, there is not a maximum number of tickets to purchase at one time. The purchaser is responsible for group ticket distribution. If you have questions, please contact HRevents@wustl.edu before purchasing. WashU Night at the Ballpark tickets are considered group sales tickets, and as such, are offered by the St. Louis Cardinals at reduced prices. All sales are final.

Each ticket holder can pick up a free WashU-branded sling bag at the ticket distribution events. Please keep in mind that the bag dimensions exceed the size limit allowed at Busch Stadium according to their bag policy.
If WashU sells enough tickets, all WashU ticket holders (including friends, family members and colleagues) will be invited to walk the pre-game warning track parade. More information will be shared via email this summer.
Ticket distribution
Group ticket sales are distributed as paper tickets per St. Louis Cardinals’ policy. Pick-up dates and locations will be shared via email and posted below. It is the employee’s responsibility to pick up tickets. You may designate someone to pick up on your behalf. Please email HRevents@wustl.edu and provide your designee’s name prior to a scheduled event.
- 6/18 at 10 a.m. – 1 p.m. | Link in the Loop lobby
- 6/20 at 11 a.m. – 3 p.m. | EPNEC, Great Room
- 7/9 at 7:30 a.m. – 12 p.m. | MCC, Training room 1404
- 7/10 at 11 a.m. – 2 p.m. | South 40, Lien House Ursa’s Fireside
- 7/16 at 7:30 a.m. – 12 p.m. | Danforth University Center (DUC) 252
- 7/17 at 10 a.m. – 3 p.m. | Barnes West County, East and West Conference Rooms
- 7/22 at 10 a.m. – 2:30 p.m. | West Campus, Room 021
- 8/6 at 1 – 4 p.m. | MCC, Training room 1404
- 8/13 at 8:30 a.m. – 2 p.m. | Danforth University Center (DUC) 276
- 8/21 at 8 a.m. – 3 p.m. | EPNEC, Great Room
- 9/6 at 8 a.m. – 2 p.m. | Link in the Loop lobby
*Note: ADA seats are limited. Based on the St. Louis Cardinals’ policy, ADA tickets are limited to two (2) tickets per group. If the group size is larger than two people, the ADA tickets will be assigned in the closest section to the remainder of the ticketed group.
Please see our FAQ for more information regarding tickets and Busch Stadium. If you have questions, please contact the HR Employee Engagement Team at HRevents@wustl.edu.
Nursery School Openings
Located on Danforth Campus, WashU’s Nursery School is enrolling for the 2024-2025 academic year and has available spaces in their 2.5 to 3-year-old class.
Their 3-Bear Summer Camp has openings for students aged 2.5 to 3 years and offers two camp sessions from June 10-28 and July 8-26.
Contact Director Nikki Scheele for details at 314-935-6689.
IT Spotlight: Reporting Phishing in the ‘New’ Outlook
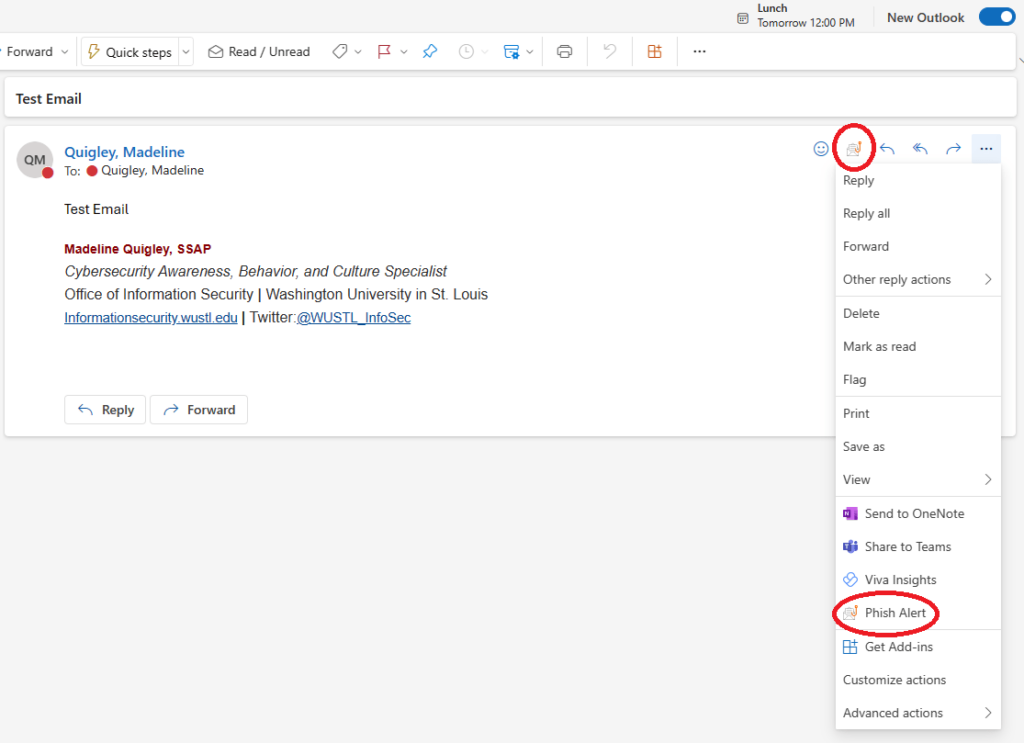
The Phish Alert Button (PAB) is one of our team’s most valuable tools for keeping the WashU community safe. When you report a phishing email using the PAB, our office will investigate the threat and take any necessary action, such as removing all similar messages from systems and notifying our community of the danger.
If you use the Outlook desktop application to monitor your email, you may have received notifications about ‘New Outlook.’ While you can still use the classic version of Outlook, you may be prompted to switch to the new version soon.
You will notice the absence of the Phish Alert Button (PAB) in this new version. In the classic version of Outlook, the PAB was in the top right-hand corner of your email, with a prominent icon in the ribbon. In the new version, the PAB is displayed a bit smaller and could be hidden in a few different places.
Please visit our Phish Alert Button (PAB) guidance page if you have trouble finding the Phish Alert Button in your email. Here, you can view several examples of the PAB and learn how to access it.
If you have trouble finding the PAB in your interface or your experience is not reflected on our guidance page, please email us at infosec@wustl.edu.
| Keep up to date with IT news at the Office of Information Security blog |
Follow the Cardiovascular Division on X!
Check out our division account, @WashUCardiology! We will be sharing division accomplishments, announcements, news, events, and more. If you have a story about the cardiovascular division that you think deserves a social media spotlight, email bolhafner@wustl.edu.